 Could this be? Fungal infection being the cause of Alzheimer's disease? Noteworthy from a recent study conducted in Spain: all the Alzheimer's disease (AD) patients had evidence of fungal infections in their brains, central nervous systems, and vascular systems, but none were found in the control subjects (those without Alzheimer's disease). Many of the symptoms of AD (such as inflammation of the central nervous system and activation of the immune system) match those with long-lasting fungal infections. A "microbial cause" has long been suggested as a cause of AD, and interestingly other studies have also found fungal infections in AD patients. The research so far has found several fungal species in AD patients (including Candida albicans). The researchers mention that in one study anti-fungal treatment reversed clinical symptoms of AD in 2 patients (but it was written off as misdiagnosis).
Could this be? Fungal infection being the cause of Alzheimer's disease? Noteworthy from a recent study conducted in Spain: all the Alzheimer's disease (AD) patients had evidence of fungal infections in their brains, central nervous systems, and vascular systems, but none were found in the control subjects (those without Alzheimer's disease). Many of the symptoms of AD (such as inflammation of the central nervous system and activation of the immune system) match those with long-lasting fungal infections. A "microbial cause" has long been suggested as a cause of AD, and interestingly other studies have also found fungal infections in AD patients. The research so far has found several fungal species in AD patients (including Candida albicans). The researchers mention that in one study anti-fungal treatment reversed clinical symptoms of AD in 2 patients (but it was written off as misdiagnosis).
Another possibility that immediately occurs to explain the findings is that perhaps Alzheimer's disease somehow results in fungal infections - that the AD makes them more prone to fungal infection. In case you're wondering - all the AD patients and control patients studied had died - this is why their brain tissue could be studied so thoroughly. Excerpts from a research article by D. Pisa et al in Nature:
Different Brain Regions are Infected with Fungi in Alzheimer’s Disease
The possibility that Alzheimer’s disease (AD) has a microbial aetiology has been proposed by several researchers. Here, we provide evidence that tissue from the central nervous system (CNS) of AD patients contain fungal cells and hyphae. Fungal material can be detected both intra- and extracellularly using specific antibodies against several fungi. Different brain regions including external frontal cortex, cerebellar hemisphere, entorhinal cortex/hippocampus and choroid plexus contain fungal material, which is absent in brain tissue from control individuals. Analysis of brain sections from ten additional AD patients reveals that all are infected with fungi. Fungal infection is also observed in blood vessels, which may explain the vascular pathology frequently detected in AD patients. Sequencing of fungal DNA extracted from frozen CNS samples identifies several fungal species. Collectively, our findings provide compelling evidence for the existence of fungal infection in the CNS from AD patients, but not in control individuals.
Neurodegenerative diseases constitute a heterogeneous group of disorders of the central nervous system (CNS) that are characterised by a slow and irreversible loss of neuronal functions. The aetiology of primary neurodegenerative diseases, such as Alzheimer’s disease (AD), multiple sclerosis (MS), Parkinson’s disease (PD) and amyotrophic lateral sclerosis (ALS), remains largely unknown. A common feature of many neurodegenerative diseases is the presence of aggregates of misfolded proteins (intracellular inclusions) in regions of the CNS that can serve as neuropathological hallmarks for disease diagnosis1,2.
Aside from cognitive decline, the vast majority of AD patients present clear signs of inflammation and damage to blood vessels15,16. Inflammation of the CNS and immune activation play a major role in the pathophysiology of AD. ... Many investigators have also considered the idea that AD is an infectious disease, or at least that infectious agents constitute a risk factor for AD21,22,23. Accordingly, genetic material from several viruses and bacteria have been reported in brains from AD patients. In particular, herpes simplex type 1 (HSV-1) and Chlamydophila pneumoniae have been suggested as potential aetiological agents of AD. In addition, brain infection by several pathogens may induce amyloid formation24,25,26. Furthermore, Αβ peptide exhibits antimicrobial activity and shows particularly strong inhibitory activity againstCandida albicans27.
Recently, we provided strong evidence for fungal infection in AD patients28,29. Fungal DNA and proteins were found in frozen brain tissue from AD patients, but not from control patient tissue. .....No fungal material was observed in brain tissue from ten control individuals, whereas fungal infection was clearly present in brains from ten additional AD patients. Moreover we were able to amplify fungal DNA from frozen tissue of different AD brain regions. Collectively, our findings provide compelling evidence for the presence of fungal infection in brains from all AD patients analysed.
Because most of the above results were obtained from only one AD patient and one control individual, it was of interest to examine CNS sections from additional AD patients and controls. To this end, we analysed ERH tissue sections from a further ten AD patients and ten controls by double immunostaining with anti-fungal (green) and anti-tubulin (red) antibodies. Notably, fungal infection was evident in all AD patients studied (Fig. 4), whereas no fungal cells were detected in tissue sections from control individuals.... The existence of different fungal morphologies reinforces the idea that several species can be present, supporting the concept of mixed fungal infections. In conclusion, fungal cells and/or hyphae were found in all AD patients analysed although the morphological characteristics may be different for each patient, thus implying that the fungal species present in each patient may also differ.
The possibility that AD is a fungal disease, or that fungal infection is a risk factor for the disease, opens new perspectives for effective therapy for these patients. The present findings demonstrate that fungi can be detected in brain tissue from different regions of the AD CNS. In all eleven patients (plus three additional CP samples) described in this study, as well as in four patients previously analysed, there is clear evidence for fungal cells inside neurons or extracellularly29. Therefore, 100% of the AD patients analysed thus far by our laboratory present fungal cells and fungal material in brain sections.....Observations from other laboratories also support the possibility of fungal infections in AD patients. .... Moreover, antifungal treatment in two patients diagnosed with AD reversed clinical symptoms51,52. The interpretation of these results was that perhaps these patients were misdiagnosed.
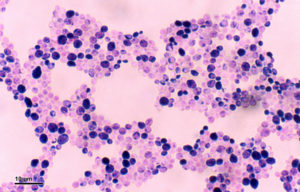 Candida albicans (Credit: Josef Reischig, Wikimedia Commons)
Candida albicans (Credit: Josef Reischig, Wikimedia Commons)
