 Probiotics are the future of sinusitis treatment. Research found that a probiotic (beneficial bacteria) that is lacking in those with chronic sinusitis, and which can successfully treat sinusitis is Lactobacillus sakei.
Probiotics are the future of sinusitis treatment. Research found that a probiotic (beneficial bacteria) that is lacking in those with chronic sinusitis, and which can successfully treat sinusitis is Lactobacillus sakei.
[See June 2022 updated version of this post.] This article is the summary of what has been learned over the past 7 years: the best L. sakei products (such as kimchi and Lanto Sinus - which can treat even the worst recurring sinus infections, frequently within days), results of people trying various L. sakei products, and other possibilities for sinus health.
Back in 2012, a study by Abreu et al suggested Lactobacillus sakei as a possible treatment for sinusitis. In the past 6 years those conclusions have been supported by the experiences of hundreds of people contacting me, and my family's experiences with L. sakei products. It really is the best sinusitis treatment for most people!
When Lactobacillus sakei works as a treatment - it can seem miraculous as sinusitis symptoms gradually disappear or greatly improve. Many times within a few days! Unfortunately it doesn't work for everyone - for a minority there seems to be no effect, and it is not clear why. It also doesn't treat seasonal allergies or allergy symptoms.
Lactobacillus sakei works best when it is used only when needed, when there are sinus symptoms. No boosters needed when feeling well! (See Treatment Summary page for different ways to use products.)
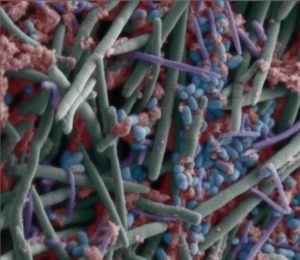
The sinus microbiome is the community of microbes (bacteria, viruses, fungi) that live in the sinuses. This community can become disrupted and imbalanced (dysbiosis) from illnesses, allergies, or antibiotics and cause a sinus infection or sinusitis.
Research in the last decade has found that not only do sinusitis sufferers lack L. sakei, they have too much of some other bacteria, and they don't have the bacteria diversity in their sinuses that healthy people without sinusitis have. There is a depletion of some bacterial species, and an increase in "abundance" of other species.
Luckily Lactobacillus sakei is found in some foods (such as some brands of live fermented kimchi), some sausage starter cultures (such as B-2), and recently in some probiotic supplements (e.g. Lanto Sinus). One reason it is used in sausage starter cultures is because L. sakei dominates over and inhibits growth of pathogenic bacteria, including Staphylococcus aureus.
BACKGROUND STORY: Seven years ago there were no probiotics containing L. sakei. None. So instead members of my family experimented using a very easy kimchi sinusitis treatment (basically dabbing and smearing kimchi at certain stages of fermentation into the nostrils like a very messy eater) and found that it cured chronic sinusitis of many years within several weeks. Obviously it contained L. sakei. It felt miraculous, especially because it was so easy to do.
After 7 years we still feel great! Because we no longer have chronic sinusitis and can easily treat sinusitis if it occurs with L. sakei, we have NOT taken antibiotics or any other bacteria killing spray or product (such as xylitol) for over 6 years. We do not use cortisone or antihistamine nasal sprays either.
WHEN A TREATMENT WORKS: Many of you have contacted me to report your own progress with various sinusitis treatments. People used terms such as "miraculous", "transformative", and "fabulous" when they had positive results with a product containing L. sakei.
When a treatment works, then all sinusitis symptoms go away or there is major improvement - frequently within a few days. Symptoms that go away include post nasal drip, sinus headaches, "clogged ears", bad breath, and sinusitis-related coughs. Even tonsil stones! (Please note: trying products to treat sinusitis is self-experimentation - effects can be positive or negative. Always be cautious. Best results are to use L. sakei only when needed.)
OVERALL RESULTS: The majority of people contacting me with results reported positive results (chronic sinusitis greatly improved or totally gone) from some form of L. sakei treatment. Successes have been from the USA, Canada, Europe, Australia, New Zealand, Japan, and Africa. Since it's from self-experimentation and not a clinical trial, I don't know the actual percentage of positive results.
Some of the people reporting success have had multiple operations, some currently have deviated septums, some with nasal polyps, and all have had long-standing chronic sinusitis, some for decades.
Chronic sinusitis sufferers also reported that the same treatments also worked to treat acute sinusitis. It seems that after colds, etc. many develop acute sinusitis again and need re-treatment (the L. sakei frequently doesn't stay in the sinuses from earlier treatments). However, the sinuses do continue improving over time, so fewer and more minimal treatments (perhaps only a few days) are needed over time.
Another very small group reported that other probiotic strains helped (but it is not always clear whether they also tried a L. sakei product), and a minority of people reported that nothing has helped and there could be a variety of reasons for this (see below). Some people reported that one product helped, but not another - whether kimchi or a L. sakei product.
THREE MAIN PRODUCT CATEGORIES: Products containing live Lactobacillus sakei which people have reported success in treating sinusitis: kimchi (and some sauerkraut), refrigerated products (e.g. Lanto Sinus), and frozen products. Note that currently the FDA does not allow any probiotics to be sold as a medical treatment – they can only be sold as a supplement.
Using the following products to treat sinusitis is self-experimentation (results are unknown and can vary). Always be cautious. (See Sinusitis Treament Summary page for methods.)
KIMCHI - Many people report that kimchi helped them. And one person  reported a homemade kimchi worked great (he was finally symptom free after many years). A few have even mentioned that kimchi has helped sinusitis with fungal problems.
reported a homemade kimchi worked great (he was finally symptom free after many years). A few have even mentioned that kimchi has helped sinusitis with fungal problems.
Kimchi brands that people reported helping their chronic sinusitis: Sunja's Kimchi (medium spicy cucumber kimchi and mild white kimchi), Sinto Gourmet brand kimchi, Mama-O's Premium Kimchi, the white Napa kimchi and cabbage kimchi made by Choi's Kimchi Company, Farmhouse Culture Kimchi, Mother-in-law's Kimchi, Ozuke Kimchi, in the United Kingdom the brand Mr Kimchi, and in Australia Kehoe's Kitchen white kimchi.
[Finding a kimchi brand with L. sakei is due to self-experimentation. The kimchi must be live, and not pasteurized. We found that kimchi may contain L. sakei from about day 14 (or earlier) to about 2 to 2 1/2 months (from the day it's made.]
When the kimchi contained L. sakei we felt the same or started feeling better within one or 2 days. If we felt more mucusy over the next 2 days, or the acute sinusitis kept getting worse, than it did not contain L. sakei. Researchers feel that it's the garlic in kimchi that encourages L. sakei growth.
SAUERKRAUT - Sauerkraut has worked for some people if it is a sauerkraut made with garlic, such as some varieties of Cleveland Kraut. Researchers feel that it's the garlic in kimchi that encourages L. sakei growth, and traditional sauerkraut typically doesn't contain garlic.
REFRIGERATED LACTOBACILLUS SAKEI PRODUCTS – A high-quality refrigerated L. sakei product specifically meant for the sinuses and treatment of sinusitis is sold by Lanto Health. The kimchi derived Lactobacillus sakei product called Lanto Sinus is meant to be used when needed. Lanto Sinus holds up well in the refrigerator, is effective, reliable, and easy to use. This product ships well because it holds up for a while (days) without refrigeration.
People have reported success using it mixed with bottled water (dabbing, smearing, spooning a little in nostrils), or swishing it dry in the mouth. I’ve been a consultant with Lanto Health on this product and have been testing and using this product successfully for over 2 years (self-experimentation!). ...continue reading "The Best Probiotic For Sinus Infections"
 It is now my eleventh year of successfully treating sinus infections with only the probiotic Lactobacillus sakei. This includes regular sinus infections, chronic sinusitis, and even when there are just a few sinus symptoms (you know, the gradual slide toward sinusitis). No antibiotics and no antibacterials in all this time! Yes, it still feels miraculous!
It is now my eleventh year of successfully treating sinus infections with only the probiotic Lactobacillus sakei. This includes regular sinus infections, chronic sinusitis, and even when there are just a few sinus symptoms (you know, the gradual slide toward sinusitis). No antibiotics and no antibacterials in all this time! Yes, it still feels miraculous!

 reported a homemade kimchi worked great (he was finally symptom free after many years). A few have even mentioned that kimchi has helped sinusitis with
reported a homemade kimchi worked great (he was finally symptom free after many years). A few have even mentioned that kimchi has helped sinusitis with 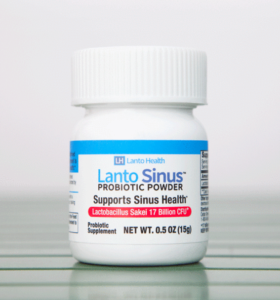 Big announcement today! The high quality product
Big announcement today! The high quality product  An amazing new study is about to start in Sweden - this study will see if "snot transplants" work for the treatment for chronic sinusitis! Will this turn out to be a permanent treatment? While
An amazing new study is about to start in Sweden - this study will see if "snot transplants" work for the treatment for chronic sinusitis! Will this turn out to be a permanent treatment? While