 Is male hair loss a risk factor for having a severe infection with COVID-19? An international group of researchers (in a joint letter in Dermatologic Therapy) hypothesize that the reason some people have severe infections of COVID-19 and others only mild symptoms, may be related to the male hormones (androgens) linked to hair loss.
Is male hair loss a risk factor for having a severe infection with COVID-19? An international group of researchers (in a joint letter in Dermatologic Therapy) hypothesize that the reason some people have severe infections of COVID-19 and others only mild symptoms, may be related to the male hormones (androgens) linked to hair loss.
"Male pattern baldness" is considered androgen-dependent hair loss and is known as androgenetic alopecia. Androgens increase in boys at puberty.
As support for their hypothesis of androgen involvement, the researchers point out that a greater proportion of men get severe COVID-19 and also die from it. They propose this possibility as an additional risk factor to consider besides the known ones of older age (over 60) and underlying conditions.
And of course they say that research is now needed to look into this possibility. In a nutshell, their hypothesis is "...the scientific evidence gives us reason to believe that beardy, bald men may be more vulnerable to COVID-19 than other individuals." At this point, who knows?
From Futurity: Hypothesis: Is COVID-19 Severity Tied to Hair Loss?
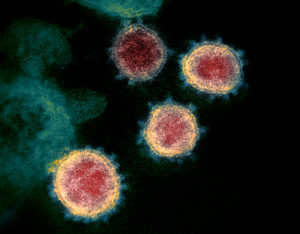
Researchers hypothesize that the same male hormones that cause hair loss may be linked to the vulnerability of patients to SARS-CoV-2, the virus that causes COVID-19.
As novel coronavirus continues its sweep across the globe, among the most confounding aspects of the pandemic has been why symptoms are so severe for some patients yet milder for many others.
Undoubtedly, age and underlying health conditions play a role—but they don’t account for fatalities among younger, otherwise healthy patients.
Physicians and scientists continue to publish data on cases, and one trend evident is that COVID-19 severity and fatalities tend to be greater among men than women. In one recent analysis of 13 US states that report numbers of deaths among men and women, men died more frequently in every case.
In a letter to the editor in the journal Dermatologic Therapy, Carlos Wambier, an assistant professor of dermatology and clinician educator at Brown University’s Warren Alpert Medical School, and other researchers lay the groundwork for their new hypothesis. Contributors to the letter are from New York University, Applied Biology, Inc., and universities in Spain, India, and Italy.
While more research is needed to test that hypothesis, Wambier says a link between androgen hormones and COVID-19 could help to explain the higher severity for men and have implications for how health care providers test and treat patients.
Here, he shares more about the journal letter and what it might mean, if confirmed, for both patients and physicians:
Q - First, can you describe the hypothesis you present in the journal? What might androgenetic alopecia—a common form of hair loss—have to do with COVID-19?
A - The main insight is that excess activation of androgens—essentially, hormones that regulate what we think of as male characteristics—is intrinsically linked to the vulnerability of patients to SARS-CoV-2. This is because the first step to the virus’s entry into a cell is a “bite” from a protease enzyme that is produced only by action of androgen hormones. The infection by SARS-CoV-2 seems to be mediated by androgens.
From a dermatological point of view, androgen receptors, which bind to DNA, have genetic variations that predispose individuals to hyperandrogenic features—the receptor binds with more affinity to the male hormones. These “hyperactive” polymorphisms are very common and cause features such as scalp hair loss (androgenetic alopecia). Other clinical signs of excess male hormone activity include high density of facial or chest hair, acne and oily skin. It is intuitive to think that if the androgen receptor is hyperactive in an individual, that person will have more of a protease called TMPRSS2 in their cell surface, too—and we’ve seen in early studies in the wake of novel coronavirus that TMPRSS2 is key to SARS-CoV-2 infection.
In other words, the scientific evidence gives us reason to believe that beardy, bald men may be more vulnerable to COVID-19 than other individuals.
Q - So the link you’re proposing could explain some of the discrepancies we’re seeing in how some patients respond to COVID-19 infect vs. others—men vs. women, for example, and fewer severe cases in children?
A - Exactly. We currently know that men have more severe COVID-19 disease and a higher rate of fatality compared to women, and we also know that children under age 10 seem extremely resistant.
Before age 10, in normal conditions, neither girls or boys have increased androgens. The first androgens start to appear during a period called adrenarche, around age 8, but those androgens produced by the adrenal glands are not very potent. After age 10 comes puberty, and androgens rise, produced by the gonads—increasing hair density in some areas, as well as oily scalp and acne. The peak of androgen production is in adult life, and they drop a little in the elderly. After menopause, women start to overexpress androgens, because of the huge drop of estrogen (female hormone), and there is an increase in facial hair and also a decrease in scalp hair density.
Taken together, this could help to explain why we’re seeing more severe and fatal COVID-19 cases in men, with a lower rate for women and very few for young children.
Q - What are the key pieces of evidence that point to the potential implication of androgens in the severity of COVID-19 cases?
A - In the journal article, we link two well-known scientific facts. First, that SARS-CoV-2 needs its spikes to be primed by the TMPRSS2 protease. Second, that the TMPRSS2 gene has only one known gene promoter, which is the androgen receptor. The gene requires androgen hormones to bind to the androgen receptor, so the cell can initiate the transcription of TMPRSS2 gene to produce the protease—a cell-surface protein that “eats” other proteins. Without this protease, host cells are not infected with SARS-CoV-2 because the virus spikes cannot bind to ACE2, a receptor implicated in COVID-19 and severe acute respiratory syndrome. The protease “eats” the spikes so they can connect to the ACE2. So more androgen activity means more proteases, which we think leads to more severe infection.
Q - In addition to hair loss, conditions like prostate gland enlargement or (for women) polycystic ovary syndrome (PCOS) are also related to androgen receptor gene. Could patients with these conditions be genetically predisposed to more severe cases of COVID-19?
A - Yes. Benign prostate enlargement is caused by a very potent androgen hormone, called DHT. This is the most potent natural androgen and it binds with great affinity to the androgen receptor—making it express proteins like TMPRSS2, which has been studied for decades in prostate health and prostate cancer research and is now known to open the door to novel coronavirus.
Women also produce DHT and testosterone, though at much lower levels than men. However, due to ovary diseases such as PCOS or ovary adenomas, women can produce very high levels of male hormones. We know PCOS is related to obesity and diabetes, so women with these conditions and post-menopausal women are likely more susceptible to severe infections, following the androgen vulnerability rationale.
Q - Can you describe the work that led you and your colleagues to identify this link? What made you, as a dermatologist, start exploring COVID-19 to begin with?
A - I’m an expert in hair biology. I like to see hair growing in the scalp of my patients—it is fun and gratifying. My colleague and coauthor, Dr. Andy Goren, is a respected scholar in hair and Minoxidil research, and we often discuss insights and new therapy for hair growth and also diagnostic tools. In recent months, we’ve explored hair genetics and polymorphisms of androgen receptors and binding sites.
Then, the pandemic came, priorities changed and instead of doing cosmetic dermatology procedures, I felt the need to contribute however possible in protecting the lives of the health care professionals, soldiers, police officers, and others who could be affected by COVID-19.
Dr. Goren and I started to share ideas about targeting the coronavirus, and since we already knew a lot about TMPRSS2 expression, we began to research other mechanisms to explain male vulnerability, including changes in pulmonary surfactant proteins (which protect against influenza) and lung cells due to male hormones. We reviewed much of the early research on COVID-19 and our journal piece synthesizes our ideas with what we learned from SARS-CoV-2 studies into the hypothesis we present.
I’m also part of a research team that will conduct a clinical trial for COVID-19 prophylaxis among volunteer health care workers in Rhode Island, where I am researching population vulnerability, with phenotype and genotype characteristics.
Q - If this link is confirmed in future studies, what are the potential implications for treating COVID-19?
A - With a new target for therapy, clinical trials could be a next step—several classes of anti-androgen drugs could hold promise for decreasing the severity of COVID-19. If confirmed, vulnerable subjects like men and women with androgenetic alopecia may be able to start prophylaxis or at least avoid risk environments for COVID-19, such as working in emergency departments or intensive care units for COVID-19 patients.
Q - What might it mean for individuals who take anabolic-androgenic steroids, whether for approved uses or otherwise?
A - In the same way the US Centers for Disease Control and Prevention recommended avoiding corticosteroids in COVID-19 patients, it might be important to avoid androgen hormones during the pandemic, particularly for police officers, health care workers, and members of the military. There’s a link in that some corticosteroids also bind to androgen receptors.
In addition, women who use progestogens for birth control that increase androgen activity (those that can cause acne or increased facial hair), might also consider contraceptive progestogens with anti-androgen activity.
Q - Your journal piece asserts the need for further study to elucidate the role of androgen receptors on the severity of COVID-19 infection. What forms might such study take? What next steps is your research team considering?
A - To test this hypothesis, it would be informative to study the epidemiology of COVID-19 patients who are predisposed to either lower or higher androgen receptor expression, such as males with androgenetic alopecia or benign prostatic hyperplasia or women with PCOS. One of my hopes is that researchers publishing information about COVID-19 cases and cohorts can add precise data on male and female patients that had severe disease or fatal outcomes. For new research, it will also be important to evaluate signs of excess male hormones—oily skin/hair, acne, facial hair, and particularly scalp hair thinning or alopecia.
In addition, our research team is considering studying polymorphisms of androgen receptor in patients that presented mild vs. severe COVID-19 disease. As a plan for that research formalizes, we’ll ultimately be looking for individuals diagnosed with COVID-19 who are willing to participate in clinical study.
Letter from Andy Goren et al., April 1, 2020, in Dermatologic Therapy: What does androgenetic alopecia have to do with COVID‐19? An insight into a potential new therapy
