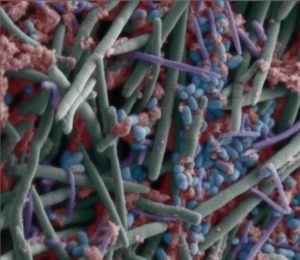
The bacteria Fusobacterium nucleatum is prevalent in periodontal disease (gum disease), but also in some chronic diseases and cancers, such as colorectal cancer. The bacteria F. nucleatum is normally found in the mouth (oral) microbiome, and its numbers increase as periodontal disease inflammation increases.
The bacteria Fusobacterium nucleatum is prevalent in periodontal disease (gum disease), but also in some chronic diseases and cancers, such as colorectal cancer. The bacteria F. nucleatum is normally found in the mouth (oral) microbiome, and its numbers increase as periodontal disease inflammation increases.
It is thought that sometimes the bacteria leaves the mouth and travels to other parts of the body, where it can promote cancer and other diseases.
A recent study found that the antibiotic FP 100 (Hygromycin A) totally eliminates the F. nucleatum bacteria in the mouth, and without causing harm to the mouth microbiome or gut microbiome. This is because it is a narrow spectrum antibiotic - only targets the harmful bacteria, and not all (both good and harmful) bacteria. While the study was only done in mice, this is promising and welcome news.
Eliminating the harmful bacteria in the mouth would potentially prevent some chronic diseases and cancers. Now we need further studies to see if this finding holds up in humans.
From Medical Xpress: First narrow-spectrum antibiotic successfully eliminates Fusobacterium nucleatum, a gum disease pathogen
In a study published in the Journal of Oral Microbiology, ADA Forsyth scientists found that FP 100 (Hygromycin A), a first-in-class, small molecule, narrow-spectrum antibiotic, successfully eradicates Fusobacterium nucleatum without harming the oral or gut microbiomes. ...continue reading "A Promising Antibiotic For Gum Disease"

 The microbes living on and in us (the human microbiome or microbiota) play a big role in our health. Certain microbes are even implicated in cancer development and progression. Thus, it shouldn't come as a surprise that new
The microbes living on and in us (the human microbiome or microbiota) play a big role in our health. Certain microbes are even implicated in cancer development and progression. Thus, it shouldn't come as a surprise that new  The incidence of both intestinal bowel diseases (IBD) and colorectal cancer is rapidly increasing in developed countries (e.g., US, Canada, Europe). There are many theories over why this is occurring, with most researchers thinking a person's diet plays a role. A big suspect in promoting IBD and colorectal cancer is the Western diet, which has lots of ultra-processed foods and is also low in fiber.
The incidence of both intestinal bowel diseases (IBD) and colorectal cancer is rapidly increasing in developed countries (e.g., US, Canada, Europe). There are many theories over why this is occurring, with most researchers thinking a person's diet plays a role. A big suspect in promoting IBD and colorectal cancer is the Western diet, which has lots of ultra-processed foods and is also low in fiber. Bottom line:
Bottom line: