It turns out that some commonly found chemicals in household products are actually hazardous to our brain health. A recent study found that these chemicals have a harmful effect on brain cells called oligodendrocytes. The harmful chemicals are quaternary compounds (found in some disinfectant products and personal care products) and some flame retardants found in household items such as furniture and electronics.
It turns out that some commonly found chemicals in household products are actually hazardous to our brain health. A recent study found that these chemicals have a harmful effect on brain cells called oligodendrocytes. The harmful chemicals are quaternary compounds (found in some disinfectant products and personal care products) and some flame retardants found in household items such as furniture and electronics.
Oligodendrocytes are cells in the central nervous system that form the myelin sheath (a layer that covers and protects nerve cells) in the brain and spinal cord. Damage to the myelin sheath underlies some neurological diseases, such as multiple sclerosis.
The researchers felt that exposure to these chemicals that damage oligodendrocytes may be a risk factor for neurological diseases. In other words, you don't want to damage these cells. Pregnant women (developing baby) and children (developing brains!) are especially vulnerable.
Bottom line: Avoid disinfecting or cleaning supplies that say they contain "quaternary compounds" and try not to buy products containing flame retardants. Check labels!
From Science Daily: Common household chemicals pose new threat to brain health, study finds
A team of researchers from the Case Western Reserve University School of Medicine has provided fresh insight into the dangers some common household chemicals pose to brain health. They suggest that chemicals found in a wide range of items, from furniture to hair products, may be linked to neurological conditions like multiple sclerosis and autism spectrum disorders. ...continue reading "Some Common Household Chemicals Have A Harmful Effect On the Brain"

 The bad news about microplastics in the environment and in all of us keeps coming. A
The bad news about microplastics in the environment and in all of us keeps coming. A  This comes under the realm of fun fact: A large
This comes under the realm of fun fact: A large  It turns out that another nasty pesticide is found in almost all of us, which we get from the foods we eat. This is the pesticide chlormequat, which is known to have harmful health effects. The use of chlormequat is on the rise in North America and Europe, where it is applied to non-organic grain crops as a plant growth regulator.
It turns out that another nasty pesticide is found in almost all of us, which we get from the foods we eat. This is the pesticide chlormequat, which is known to have harmful health effects. The use of chlormequat is on the rise in North America and Europe, where it is applied to non-organic grain crops as a plant growth regulator. Unfortunately, unprocessed and minimally processed foods are more expensive than ultra-processed foods. So it wasn't surprising that socioeconomic levels (including income levels) made a difference - the lower the household income, the greater the average ultra-processed food intake.
Unfortunately, unprocessed and minimally processed foods are more expensive than ultra-processed foods. So it wasn't surprising that socioeconomic levels (including income levels) made a difference - the lower the household income, the greater the average ultra-processed food intake. There appears to be a big downside to an all plant diet, which is the possibility of missing essential nutrients that are found in dairy and meat (e.g., vitamin B12, vitamin D3, iron, zinc, choline).
There appears to be a big downside to an all plant diet, which is the possibility of missing essential nutrients that are found in dairy and meat (e.g., vitamin B12, vitamin D3, iron, zinc, choline).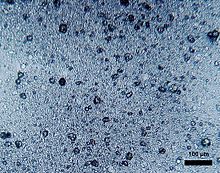
 A recent small
A recent small