Not all cleaning products or chemicals used in dry cleaning are safe to use. A recent study found that the chemical tetrachloroethylene (PERC or PCE) can cause serious liver harm in the form of liver fibrosis, and that the effects are dose dependent for liver fibrosis. The more a person is exposed, the greater the risk of developing liver fibrosis.
PERC is a chemical that used to be found in household products, such as spot removers, furniture stripper, adhesive glues, suede protectors, spray-on water repellents, but is being phased out. It is also commonly used in dry cleaning of clothing, and it has 10 years to phase out. It will continue to be used in a number of industrial settings, for example, as a degreaser. Tetrachloroethylene (PERC) is a volatile organic compound (VOC).
Liver fibrosis is the buildup of tough scar tissue in the liver resulting from chronic inflammation and persistent damage. Unfortunately, over time this scarring can progress to liver failure or liver cancer.
Bottom line: Avoid products with PERC. The danger is in inhaling the chemical's fumes or getting it on your skin (contact with the chemical). Nowadays PERC is mainly used in industrial settings (resulting in occupational exposure). It is being phased out in consumer products and dry cleaning because it is a carcinogen (cancer causing).
From Science Daily: Hidden household toxin triples liver disease risk, study finds
Liver disease most often develops due to one of three major causes: excessive alcohol use, the buildup of fat in the liver associated with obesity, diabetes, and high cholesterol, or viral infections such as hepatitis B and C.
Researchers from Keck Medicine of USC have identified another potential cause of liver damage. A new study published in Liver International links tetrachloroethylene (PCE), a chemical widely used in dry cleaning and found in household products like adhesive glues, spot removers, and stainless steel polish, to serious liver harm. ...continue reading "Chemical Exposure Linked to Liver Scarring"

 There is much concern over the amounts of microplastics and nanoplastics in the environment, especially since they are turning up wherever we look. Including inside
There is much concern over the amounts of microplastics and nanoplastics in the environment, especially since they are turning up wherever we look. Including inside 
 Big snow event in the northeast earlier this week.
Big snow event in the northeast earlier this week.

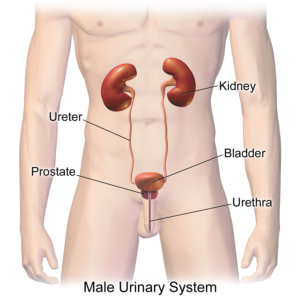
 The researchers viewed physical activity as having reno-protective effects - in both the general population and in persons with CKD. This is because it lowers the risk of developing CKD, but it also slows kidney function decline. By the way, other
The researchers viewed physical activity as having reno-protective effects - in both the general population and in persons with CKD. This is because it lowers the risk of developing CKD, but it also slows kidney function decline. By the way, other  Not only humans and many foods (e.g., fruits) have microbiomes - the community of bacteria, viruses, archaea, and fungi living on and in the organism.
Not only humans and many foods (e.g., fruits) have microbiomes - the community of bacteria, viruses, archaea, and fungi living on and in the organism.  Organic food sales in the USA are up, up, up - yet it turns out that organic farmland in the United States is shrinking. The decrease in organic acreage is approximately 1.5 million acres from 2021 to 2023. Yet, in 2024,
Organic food sales in the USA are up, up, up - yet it turns out that organic farmland in the United States is shrinking. The decrease in organic acreage is approximately 1.5 million acres from 2021 to 2023. Yet, in 2024,  An excellent group to support is the
An excellent group to support is the