
Once again, a recent study found that daily consumption of coffee has health benefits.
Recent research found that drinking a moderate amount of coffee (2 to 3 cups of daily) or 1 to 2 cups of tea daily was associated with a lower risk of dementia and better cognitive function. Decaf coffee appeared to have no effect on risk of dementia or cognitive functioning.
Persons with the highest intake (2 to 3 cups or more daily) of caffeinated coffee had an 18% lower risk of dementia compared with those who drank little or no caffeinated coffee. The large study followed people for as long as 43 years.
From Medical Xpress: Consuming 2–3 cups of coffee daily associated with lower dementia risk, better cognitive function
A new prospective cohort study by investigators from Mass General Brigham, Harvard T.H. Chan School of Public Health, and the Broad Institute of MIT and Harvard analyzed 131,821 participants from the Nurses' Health Study (NHS) and Health Professionals Follow-Up Study (HPFS), finding that moderate consumption of caffeinated coffee (two to three cups a day) or tea (one to two cups a day) reduced dementia risk, slowed cognitive decline, and preserved cognitive function. ...continue reading "Consuming Coffee Or Tea Daily Associated With Lower Risk of Dementia"


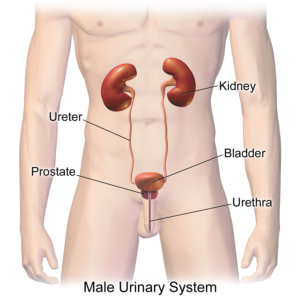
 The researchers viewed physical activity as having reno-protective effects - in both the general population and in persons with CKD. This is because it lowers the risk of developing CKD, but it also slows kidney function decline. By the way, other
The researchers viewed physical activity as having reno-protective effects - in both the general population and in persons with CKD. This is because it lowers the risk of developing CKD, but it also slows kidney function decline. By the way, other  Not only humans and many foods (e.g., fruits) have microbiomes - the community of bacteria, viruses, archaea, and fungi living on and in the organism.
Not only humans and many foods (e.g., fruits) have microbiomes - the community of bacteria, viruses, archaea, and fungi living on and in the organism.  Organic food sales in the USA are up, up, up - yet it turns out that organic farmland in the United States is shrinking. The decrease in organic acreage is approximately 1.5 million acres from 2021 to 2023. Yet, in 2024,
Organic food sales in the USA are up, up, up - yet it turns out that organic farmland in the United States is shrinking. The decrease in organic acreage is approximately 1.5 million acres from 2021 to 2023. Yet, in 2024,  An excellent group to support is the
An excellent group to support is the 


 Scientists have long known about some factors linked to a higher risk of developing multiple sclerosis (MS).These include low levels of sunlight exposure, low vitamin D blood levels, smoking, and being infected with the Epstein Barr virus in adolescence and adulthood (infectious mononucleosis). Recent
Scientists have long known about some factors linked to a higher risk of developing multiple sclerosis (MS).These include low levels of sunlight exposure, low vitamin D blood levels, smoking, and being infected with the Epstein Barr virus in adolescence and adulthood (infectious mononucleosis). Recent  The microbes in your mouth may offer a clue to obesity. New
The microbes in your mouth may offer a clue to obesity. New