 For years scientists have warned of breast cancer links to some pesticides, while the EPA and the chemical industry pooh-poohed these associations. Just a coincidence, not true, studies poorly done, and ignore or attack were their common responses. Seeing a mismatch between scientific evidence and what the EPA was saying led researchers at the respected Silent Spring Institute to examine EPA pesticide documents and studies.
For years scientists have warned of breast cancer links to some pesticides, while the EPA and the chemical industry pooh-poohed these associations. Just a coincidence, not true, studies poorly done, and ignore or attack were their common responses. Seeing a mismatch between scientific evidence and what the EPA was saying led researchers at the respected Silent Spring Institute to examine EPA pesticide documents and studies.
The big question: was the EPA deliberately ignoring evidence that some pesticides can cause mammary tumors (the equivalent of breast cancer in humans)? In other words, was the EPA ignoring evidence of some pesticides being carcinogenic when they were determining how to classify a pesticide and its risk assessment?
Their finding: Yes, the EPA was ignoring evidence for a number of pesticides causing mammary tumors. And because of this some pesticides are not labeled as cancer-causing (carcinogenic) by the FDA. Another problem they (and others) found is that the EPA is ignoring evidence about endocrine disruptors, and evidence that some chemicals have a bigger effect at smaller doses than big doses. The old view: the dose makes the poison, but now we know that doesn’t apply to endocrine disruptors which may have a bigger effect at smaller doses.
The scientists identified 28 pesticides that produced mammary tumors in studies, but the EPA acknowledged tumors only in nine, and dismissed the rest. The scientists strongly suggested that the EPA reassess cancer risks for some commonly used pesticides, including malathion, triclopyr, atrazine, propylene oxide, and 3-iodo-2-propynyl butylcarbamate (IPBC).
Another concerning problem (and not addressed at all by the EPA) is that 10 pesticides had reported effects on the mammary gland (other than tumors). For five of these pesticides (atrazine, chlorpyrifos, malathion, methoxychlor, and parathion) exposure during pregnancy or early life altered mammary gland development. What does this mean long-term? Will there be effects on lactation (breast-feeding)? (Some research suggests yes).
From Medical Xpress: Dozens of pesticides linked with mammary gland tumors in animal studies
In an analysis of how regulators review pesticides for their potential to cause cancer, researchers at Silent Spring Institute identified more than two dozen registered pesticides that were linked with mammary gland tumors in animal studies. The new findings raise concerns about how the US Environmental Protection Agency (EPA) approves pesticides for use and the role of certain pesticides in the development of breast cancer.
Several years ago, a resident on Cape Cod in Massachusetts contacted researchers at Silent Spring looking for information on an herbicide called triclopyr. Utility companies were looking to spray the chemical below power lines on the Cape to control vegetation. ...continue reading "EPA Needs to Look At Breast Cancer Risks From Pesticides"
 Most Americans eat highly processed or ultra-processed foods every single day, with most of their daily calories from them! There are all sorts of health risks from these foods, with a recent study finding an overall increased risk of cancer, as well as prostate and breast cancer.
Most Americans eat highly processed or ultra-processed foods every single day, with most of their daily calories from them! There are all sorts of health risks from these foods, with a recent study finding an overall increased risk of cancer, as well as prostate and breast cancer.
 People worry about breast cancer and whether exposure to chemicals "in the environment" can lead to breast cancer. According to many studies the answer is: YES, absolutely - and this is why they are called carcinogens (a substance capable of causing cancer). What are the chemicals?
People worry about breast cancer and whether exposure to chemicals "in the environment" can lead to breast cancer. According to many studies the answer is: YES, absolutely - and this is why they are called carcinogens (a substance capable of causing cancer). What are the chemicals? Also, avoid using pesticides as much as possible, and instead use least toxic Integrated Pest Management (IPM) or organic methods, both inside the home and outside.
Also, avoid using pesticides as much as possible, and instead use least toxic Integrated Pest Management (IPM) or organic methods, both inside the home and outside. Do you know what chemicals you're exposed to on a daily basis? A recent study found that women with cancers of the breast, uterus, skin (melanoma), or ovaries had significantly higher levels of certain endocrine disrupting chemicals in their bodies than women without any of those cancers.
Do you know what chemicals you're exposed to on a daily basis? A recent study found that women with cancers of the breast, uterus, skin (melanoma), or ovaries had significantly higher levels of certain endocrine disrupting chemicals in their bodies than women without any of those cancers. Some dietary supplements can do serious harm, especially when taken in high doses. A
Some dietary supplements can do serious harm, especially when taken in high doses. A 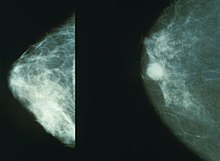
 We all know that microbes (fungi, viruses, bacteria) live throughout our bodies - this is the human microbiome or microbiota. What is really interesting is that cancer tumors also have microbiomes (tumor microbiome), and these microbial communities are different than that found in healthy people (without tumors).
We all know that microbes (fungi, viruses, bacteria) live throughout our bodies - this is the human microbiome or microbiota. What is really interesting is that cancer tumors also have microbiomes (tumor microbiome), and these microbial communities are different than that found in healthy people (without tumors). We've all been warned over and over to avoid sunlight in order to avoid skin cancer, but... conflicting with that advice are studies linking higher sunlight exposure to lower levels of other cancers,
We've all been warned over and over to avoid sunlight in order to avoid skin cancer, but... conflicting with that advice are studies linking higher sunlight exposure to lower levels of other cancers,  For years scientists have warned of breast cancer links to some pesticides, while the EPA and the chemical industry pooh-poohed these associations. Just a coincidence, not true, studies poorly done, and ignore or attack were their common responses. Seeing a mismatch between scientific evidence and what the EPA was saying led researchers at the respected Silent Spring Institute to examine EPA pesticide documents and studies.
For years scientists have warned of breast cancer links to some pesticides, while the EPA and the chemical industry pooh-poohed these associations. Just a coincidence, not true, studies poorly done, and ignore or attack were their common responses. Seeing a mismatch between scientific evidence and what the EPA was saying led researchers at the respected Silent Spring Institute to examine EPA pesticide documents and studies.