 Once again artificial sweeteners are in the news, and not in a good way. New research found that the sugar substitute erythritol, at a concentration typically found in an artificially sweetened beverage, has harmful effects on the small blood vessels of the brain.
Once again artificial sweeteners are in the news, and not in a good way. New research found that the sugar substitute erythritol, at a concentration typically found in an artificially sweetened beverage, has harmful effects on the small blood vessels of the brain.
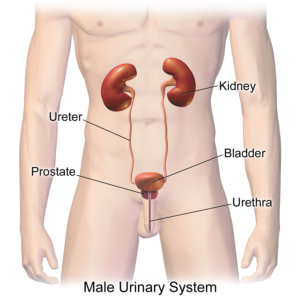
Erythritol crosses the blood brain barrier and interacts with the brain's cerebrovasculature (the blood vessels in the brain, including the arteries, veins, and capillaries that supply blood and nutrients to the brain tissue). This study focused on the smallest blood vessels (microvascular) in the brain. And yes, found that the amount or erythritol in 1 diet beverage has adverse effects at a cellular level on these blood vessels.
This study was done in a lab setting (and not directly on humans), but research results match up with other studies on erythritol. Other studies already found that erythritol increases the risk of heart attacks, heart disease, strokes, as well as blood clot formation. This study's results give an explanation for why there is a increased risk of these brain vascular (blood vessel) events happening.
Erythritol is found in some beverages advertised as low or zero calorie (e.g., Monster Zero energy drinks, Blue Sky Zero Sugar soda, Red Bull Zero) and in some low calorie foods (e.g., Halo Top low-calorie ice cream). Read ingredient lists on labels!
From Medical Xpress: Major sugar substitute found to impair brain blood vessel cell function, posing potential stroke risk
Erythritol may impair cellular functions essential to maintaining brain blood vessel health, according to researchers at the University of Colorado Boulder. Findings suggest that erythritol increases oxidative stress, disrupts nitric oxide signaling, raises vasoconstrictive peptide production, and diminishes clot-dissolving capacity in human brain microvascular endothelial cells. ...continue reading "The Sugar Substitute Erythritol And the Brain’s Blood Vessels"


 Remember when for years eating eggs was viewed as unhealthy? And people were told to only eat egg whites? Well, well... how views have changed. Another recent
Remember when for years eating eggs was viewed as unhealthy? And people were told to only eat egg whites? Well, well... how views have changed. Another recent 
 One message keeps being supported by research: Eat a diet rich in fruits, vegetables, seeds, nuts, whole grains, legumes, and olive oil. A reason is because this diet is anti-inflammatory. And it turns out that inflammation is at the root of many diseases, including heart disease. And dementia.
One message keeps being supported by research: Eat a diet rich in fruits, vegetables, seeds, nuts, whole grains, legumes, and olive oil. A reason is because this diet is anti-inflammatory. And it turns out that inflammation is at the root of many diseases, including heart disease. And dementia. The artificial sweetener erythritol is added to many foods. However, this sugar substitute (which is often blended with stevia) may cause health problems . A recent small
The artificial sweetener erythritol is added to many foods. However, this sugar substitute (which is often blended with stevia) may cause health problems . A recent small  Eating plant-based foods has health benefits. But only if it's from real foods, and not ultra-processed. A recent
Eating plant-based foods has health benefits. But only if it's from real foods, and not ultra-processed. A recent 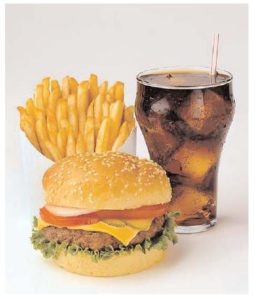 The incidence of both intestinal bowel diseases (IBD) and colorectal cancer is rapidly increasing in developed countries (e.g., US, Canada, Europe). There are many theories over why this is occurring, with most researchers thinking a person's diet plays a role. A big suspect in promoting IBD and colorectal cancer is the Western diet, which has lots of ultra-processed foods and is also low in fiber.
The incidence of both intestinal bowel diseases (IBD) and colorectal cancer is rapidly increasing in developed countries (e.g., US, Canada, Europe). There are many theories over why this is occurring, with most researchers thinking a person's diet plays a role. A big suspect in promoting IBD and colorectal cancer is the Western diet, which has lots of ultra-processed foods and is also low in fiber. The ingredient xylitol is added to a number of products, but recent studies find it to have no health benefits (
The ingredient xylitol is added to a number of products, but recent studies find it to have no health benefits (