 It is now my twelfth year of successfully treating sinus infections with only the probiotic Lactobacillus sakei. My twelfth year! This includes regular sinus infections, my initial chronic sinusitis, and even when there are just a few sinus symptoms (you know, the gradual slide toward sinusitis).
It is now my twelfth year of successfully treating sinus infections with only the probiotic Lactobacillus sakei. My twelfth year! This includes regular sinus infections, my initial chronic sinusitis, and even when there are just a few sinus symptoms (you know, the gradual slide toward sinusitis).
Amazingly, no antibiotics and no antibacterials in all this time! Just using a product with the beneficial bacteria L. sakei when needing it is all it takes. To say it feels miraculous is an understatement.
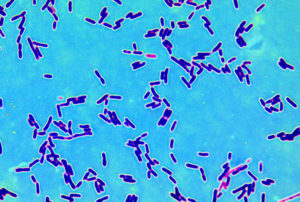
Studies show that the beneficial bacteria Lactobacillus sakei occurs naturally (in tiny amounts) in healthy sinuses, but is depleted or missing in those with sinusitis. It is normal for a community of bacteria, viruses, fungi to live in the sinuses - this is the sinus microbiome.
My journey started in the winter of 2013 after reading research in late 2012 about L. sakei. I started with kimchi back then, but in the last few years I've used the product Lanto Sinus, which contains a kimchi-derived strain of Lactobacillus sakei.
In the past decade, I have heard from hundreds of people from all over the world, and the majority agree that L. sakei works great as a sinus treatment! Other probiotic species just don't work, even though they may help with some symptoms. [See Best Probiotics For Sinusitis for details on results and products used.]
Lessons Learned Over the Past Eleven Years:
1) Lactobacillus sakei alone is enough to treat sinus infections or sinusitis. It helps with all the associated symptoms: mucus dripping down the throat (post-nasal drip), sinus pressure, sinus headaches, earaches and coughs from sinusitis, etc.
2) Using L. sakei (whether in kimchi or Lanto Sinus) should take about a minute! No fancy methods or protocols needed.
3) Only use L. sakei when needed. This means when there are sinus symptoms (e.g., lots of mucus, post nasal drip) or you're sliding towards sinusitis. No need to wait till the sinus infection is full-blown.
4) Stop using it when feeling better. Don't use it daily or as a preventive, but only when needed. There are many species of microbes living in the sinuses, so you don't want to flood the sinuses with just one species for weeks on end.
5) After using it for a few days, evaluate whether you can stop or whether you need to keep using it longer. The sinuses frequently keep improving and rebalancing after stopping L. sakei. One can always use more if needed.
6) People use L. sakei products (e.g., Lanto Sinus) all sorts of ways. Can mix the powder with bottled/sterile water and dab/smear in nostrils (regular use). Or swish alone in the mouth - a gentle and cautious method. Or use it with saline nasal irrigation - a strong way to use. Yes, you can use less than the recommended dosage.
Please note: The only way kimchi (the juice) has an effect is by dabbing or smearing a little in the nostrils.
7) Don't overdo it. Using a little bit in the nostrils (as described in Sinusitis Treatment Summary) is sufficient. Let the little buggers travel on their own throughout the sinuses!
8) L. sakei normally lives in healthy sinuses, which is why it is such an effective sinus infection treatment for so many people. L. sakei overpowers or dominates over harmful (pathogenic bacteria), and so researchers are now studying its use for a variety of health conditions.
9) Over time a person typically needs less L. sakei to treat sinus symptoms. The L. sakei colonizes in the sinuses (can be short-term or long-term). Weeks or months can go by without needing to use it again.
10) When L. sakei works for a person, it can feel miraculous as sinusitis symptoms disappear, frequently within a few days. Others have slower improvement. Unfortunately, it doesn't work for everyone and only self-experimentation determines whether it does and how best to use it.
11) It is OK to do ordinary nasal irrigation once or twice a day on same day as using L. sakei product. Also OK, if needed, are nasal corticosteroids (e.g., Flonase), decongestants (e.g., Sudafed), and guaifenesin (e.g., Mucinex).
12) Every person's sinus and respiratory microbiome is a little different, which is why finding what works for a person is self-experimentation.
13) After using L. sakei in any product (e.g., kimchi) for an extended time, can start feeling like it's not working well anymore or some sinus symptoms may appear (e.g., mucus). This could be overuse or too much of a product - that is, flooding the respiratory system with too much of whatever you're using, and now need to add a little bit of other beneficial bacteria.
Simply stop using the product and try adding some other microbes into the respiratory system for a day or two or even more if needed - this will help rebalance the sinuses. Open a multistrain probiotic capsule and swish the powder in the mouth. [See Sinusitis Treatment Summary] Lactobacillus and Bifidobacterium species are OK to use - they are normally found in our bodies in tiny amounts.
This first happened in 2013 when I kept using kimchi even when sinuses felt healthy - I thought I needed a boost several times a week. Nope. After many months I started developing sinus symptoms and only switching to a different type of kimchi got rid of the symptoms. Over the years I've done this with every L. sakei product, and adding other microbes for a day or more solved the problem, and I could go back to the original product when next needed.
14) One possibility why sinus infections keep occurring over the years, even if less frequently, is because other bacterial species are also diminished in those with sinus infections (as shown by sinus microbiome studies). And these species are not available in probiotics.
15) People report that using L. sakei has helped bacterial conditions other than sinusitis. This includes earaches, coughs (bronchitis), tonsil stones. Sounds like lots of self-experimentation going on!
Good health!

 This month a number of persons asked me about the probiotic Lactococcus lactis (in Probiorinse) and whether it works. This product is marketed to people with sinusitis or sinus infections, with the message that it improves the sinus microbiome and sinus health. Does it?
This month a number of persons asked me about the probiotic Lactococcus lactis (in Probiorinse) and whether it works. This product is marketed to people with sinusitis or sinus infections, with the message that it improves the sinus microbiome and sinus health. Does it? Researchers are starting to raise concerns about routine daily intake of probiotics for "gut health". Much is still unknown, but problems are starting to appear. A healthy gut contains hundreds of species (bacteria, fungi, viruses), and taking megadoses of a few species (a probiotic supplement) can overwhelm the normal gut microbial community. A healthy gut is one with a greater diversity of species, not just some species.
Researchers are starting to raise concerns about routine daily intake of probiotics for "gut health". Much is still unknown, but problems are starting to appear. A healthy gut contains hundreds of species (bacteria, fungi, viruses), and taking megadoses of a few species (a probiotic supplement) can overwhelm the normal gut microbial community. A healthy gut is one with a greater diversity of species, not just some species.