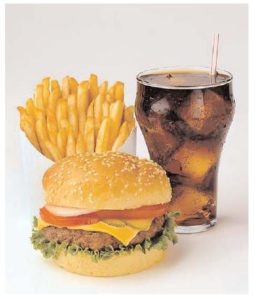
 The incidence of both intestinal bowel diseases (IBD) and colorectal cancer is rapidly increasing in developed countries (e.g., US, Canada, Europe). There are many theories over why this is occurring, with most researchers thinking a person's diet plays a role. A big suspect in promoting IBD and colorectal cancer is the Western diet, which has lots of ultra-processed foods and is also low in fiber.
The incidence of both intestinal bowel diseases (IBD) and colorectal cancer is rapidly increasing in developed countries (e.g., US, Canada, Europe). There are many theories over why this is occurring, with most researchers thinking a person's diet plays a role. A big suspect in promoting IBD and colorectal cancer is the Western diet, which has lots of ultra-processed foods and is also low in fiber.
A recent large study looked at 6 major diets and how they impact the gut microbiome. The six dietary patterns were: Western diet, Mediterranean diet, high-fiber diet, plant-based diet, high protein diet, and ketogenic diet.
And surprise, surprise - eating a Western diet resulted in having an increase in gut bacterial species linked to chronic inflammation, heart disease, colorectal cancer, IBD, and diabetes. The Mediterranean style diet had an increase in bacterial species linked to a lower risk of cardiovascular disease, IBD, and type 2 diabetes. In fact, all 6 diets had distinct bacterial profiles in the gut.
 Bottom line: The foods a person eats can either feed and nourish beneficial bacteria or harmful bacteria (linked to cancer and IBD). Best for health is a Mediterranean style diet (lots of fruits, vegetables, whole grains, legumes, seeds, nuts), and avoiding ultra-processed foods. You are what you eat!
Bottom line: The foods a person eats can either feed and nourish beneficial bacteria or harmful bacteria (linked to cancer and IBD). Best for health is a Mediterranean style diet (lots of fruits, vegetables, whole grains, legumes, seeds, nuts), and avoiding ultra-processed foods. You are what you eat!
From Medical Xpress: Western diets pose greater risk of cancer and inflammatory bowel disease, study finds
Western diets pose a greater risk of inflammatory bowel disease (IBD) and colorectal cancer, according to a milestone review of what people eat around the world. ...continue reading "A Mediterranean Style Diet Feeds Beneficial Gut Bacteria"


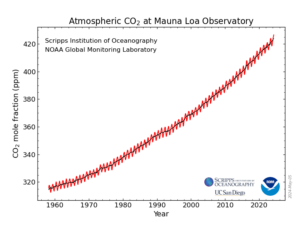
 Uh-oh. The Earth is really warming up, and very rapidly. Sunday was the
Uh-oh. The Earth is really warming up, and very rapidly. Sunday was the  Studies on aspirin keep coming. For decades, studies found that persons taking aspirin frequently have a lowered risk of developing colorectal (colon) cancer, and that they are less likely to die if they do develop colorectal cancer. A recent
Studies on aspirin keep coming. For decades, studies found that persons taking aspirin frequently have a lowered risk of developing colorectal (colon) cancer, and that they are less likely to die if they do develop colorectal cancer. A recent  This year a number of persons reported to me that when their neighbors started with mosquito and tick control pesticide applications, they no longer have bees or butterflies in their yards. Even if they have lots of bee and butterfly friendly flowers, or lots of clover - they now rarely or never see bees and butterflies. This has also been my experience.
This year a number of persons reported to me that when their neighbors started with mosquito and tick control pesticide applications, they no longer have bees or butterflies in their yards. Even if they have lots of bee and butterfly friendly flowers, or lots of clover - they now rarely or never see bees and butterflies. This has also been my experience. Bees are pollinators
Bees are pollinators A recent large
A recent large 
 Great news for individuals with lower back pain. Which is a lot of us. A recent
Great news for individuals with lower back pain. Which is a lot of us. A recent  The CDC currently
The CDC currently  Tick-borne encephalitis is a serious viral infection of the central nervous system. It starts out with symptoms such as fever, headaches, chills, but
Tick-borne encephalitis is a serious viral infection of the central nervous system. It starts out with symptoms such as fever, headaches, chills, but