 For a while now it's known that exposure to pesticides is associated with developing Parkinson's Disease. But which pesticides? This is an important question because millions of pounds of pesticides are applied in the US each year. A recent study provides some answers.
For a while now it's known that exposure to pesticides is associated with developing Parkinson's Disease. But which pesticides? This is an important question because millions of pounds of pesticides are applied in the US each year. A recent study provides some answers.
The Harvard and UCLA Health researchers looked at 288 pesticides. They found that 53 pesticides were associated with Parkinson's disease, but 10 were directly toxic to dopaminergic neurons. Dopaminergic neurons are cells in the brain, and their degeneration and death play a key role in Parkinson's disease.
The 10 most toxic pesticides included four insecticides (dicofol, endosulfan, naled, propargite), three herbicides (diquat, endothall, trifluralin), and three fungicides (copper sulfate [basic and pentahydrate] and folpet). Some are commonly used even by homeowners, such as Preen (contains trifluralin) and Ortho Groundclear (contains diquat).
They also found that co-exposure to several pesticides (which typically happens) have a greater negative effect than just 1 pesticide.
Bottom line: There is much we don't know about pesticides, but studies are finding more health harms each year. Avoid using pesticides in your home, lawn, and garden if you can - especially unnecessary "cosmetic" lawn pesticides. Best and safest is to use nontoxic Integrated Pest Management (IPM) or organic.
Think of it this way: pesticides can give you cancer and damage your health, but clover and crabgrass can't.
From Science Daily: 10 pesticides toxic to neurons involved in Parkinson's
Researchers at UCLA Health and Harvard have identified 10 pesticides that significantly damaged neurons implicated in the development of Parkinson's disease, providing new clues about environmental toxins' role in the disease. ...continue reading "Pesticides Involved in the Development of Parkinson’s Disease"


 Study after study finds all sorts of negative health effects from exposure to pesticides, including cancers, endocrine (hormone) disruption, and neurological effects. Pesticide exposures can occur in the home, at work or school, in the air (drift), and in food and water. A
Study after study finds all sorts of negative health effects from exposure to pesticides, including cancers, endocrine (hormone) disruption, and neurological effects. Pesticide exposures can occur in the home, at work or school, in the air (drift), and in food and water. A  Many pesticides are neurotoxins. Dr. Ray Dorsey (publisher of
Many pesticides are neurotoxins. Dr. Ray Dorsey (publisher of  New
New  A
A 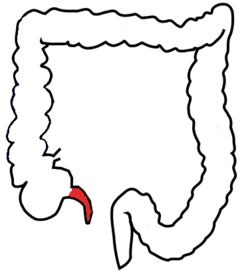 A benefit (perhaps) of having the appendix taken out in childhood - it is associated with a lower rate of Parkinson's disease decades later in life, according to an
A benefit (perhaps) of having the appendix taken out in childhood - it is associated with a lower rate of Parkinson's disease decades later in life, according to an