 There used to be alternative medicine, but it has evolved to what is now called integrative medicine. There are integrative centers even at some if the most prestigious medical institutions in the USA (Harvard, Mayo Clinic,etc). Integrative medicine is part of the medical establishment, so there is an emphasis on treatments that can be scientifically investigated, and conventional medical treatments are also used as needed. But there is a concern with wellness, with looking at the whole body, at prevention and treating chronic diseases (such as heart disease and diabetes) that take years to develop and are tied to the ways people think, feel, and live their everyday lives (so they look at stress, diet, lifestyles).
There used to be alternative medicine, but it has evolved to what is now called integrative medicine. There are integrative centers even at some if the most prestigious medical institutions in the USA (Harvard, Mayo Clinic,etc). Integrative medicine is part of the medical establishment, so there is an emphasis on treatments that can be scientifically investigated, and conventional medical treatments are also used as needed. But there is a concern with wellness, with looking at the whole body, at prevention and treating chronic diseases (such as heart disease and diabetes) that take years to develop and are tied to the ways people think, feel, and live their everyday lives (so they look at stress, diet, lifestyles).
What I especially like is the quote taught in medical schools: “A common homily we tell our students is that in five years, half of what we taught them will be wrong. We just don’t know which half.” That alone is a good reason for a person to take responsibility for living the most healthy lifestyle that they can (to focus on wellness and prevention), rather than depending on medicines for "treatments" and "cures". Excerpts from The Atlantic:
The Evolution of Alternative Medicine
Back in the 1990s, the word “alternative” was a synonym for hip and forward-thinking.... That was the decade when doctors started to realize just how many Americans were using alternative medicine, starting with a 1993 paper published in The New England Journal of Medicine. The paper reported that one in three Americans were using some kind of “unconventional therapy.” Only 28 percent of them were telling their primary-care doctors about it.
Enough Americans had similar interests that, in the early 1990s, Congress established an Office of Alternative Medicine within the National Institutes of Health. Seven years later, that office expanded into the National Center for Complementary and Alternative Medicine (NCCAM), with a $50 million budget dedicated to studying just about every treatment that didn’t involve pharmaceuticals or surgery—traditional systems like Ayurveda and acupuncture along with more esoteric things like homeopathy and energy healing.Some thought the NCCAM’s work was too far outside the mainstream....
In an email, Briggs confirmed that her center’s mission has shifted over the years...”That change became more pronounced a few months ago, when Congress removed the word “alternative” from the NCCAM’s name, redubbing it the National Center for Complementary and Integrative Health (NCCIH).
The idea of alternative medicine—an outsider movement challenging the medical status quo—has fallen out of favor since my youth. Plenty of people still identify strongly with the label, but these days, they’re often the most extreme advocates, the ones who believe in using homeopathy instead of vaccines, “liver flushes” instead of HIV drugs, and garlic instead of chemotherapy. In contrast, integrative doctors see themselves as part of the medical establishment. “I don’t like the term ‘alternative medicine,’” says Mimi Guarneri, a longtime cardiologist and researcher who founded the Academy of Integrative Health and Medicine as well as the integrative center at Scripps.
After visiting the NIH center and talking to leading integrative physicians, I can say pretty definitively that integrative health is not just another name for alternative medicine. There are 50 institutions around the country that have integrative in their name, at places like Harvard, Stanford, Duke, and the Mayo Clinic. Most of them offer treatments like acupuncture, massage, and nutrition counseling, along with conventional drugs and surgery.
The actual treatments they use vary, but what ties integrative doctors together is their focus on chronic disease and their effort to create an abstract condition called wellness. In the process, they’re scrutinizing many therapies that were once considered alternative, subjecting them to the scientific method and then using them the same way they’d incorporate any other evidence-based medicine.
It’s hard to talk about integrative health without using abstract terms like wellness, vitality, and healing...For a long time, though, the medical profession was so busy treating acute illness that it didn’t put as much attention on preventing heart disease, diabetes, or cancer...The bigger problem, says Hyman, is that most doctors aren’t well equipped to treat chronic disease. “We have an acute-disease system for a chronic-disease population,” he told me. “The whole approach is to suppress and inhibit the manifestations of disease.”
The question is how integrative doctors try to restore balance—and the answer varies. Many of them focus on diet to a degree that goes far beyond the usual guidelines about avoiding salt or trans fat. They’ll look for undiagnosed food sensitivities or hormonal imbalances, with the idea that these problems account for many chronic health complaints and cause even more serious breakdowns over time. There’s a lot of emphasis on intestinal bacteria. “We now know that so many separate things are linked to what’s going on in the gut,” Hyman told me, alluding to a growing body of literature linking the microbiome to everything from cancer to mood disorders. Guarneri, the cardiologist who founded the integrative center at Scripps, told me integrative health is highly personalized.
Integrative doctors tend to favor treatments that are—as Briggs, the NCCIH director, put it—“amenable to scientific investigation.” Several of the doctors I interviewed told me they don’t prescribe homeopathic remedies, for instance, because there’s no evidence to support them....When integrative doctors do employ alternative-seeming treatments, it’s usually to manage pain or reduce stress.
Aside from these variations, there’s another reason it’s hard to define integrative health: It doesn’t exist in a vacuum. Its practitioners are part of the same medical establishment as other doctors, going to the same conferences and publishing in the same journals. They’ve influenced and been influenced by major trends in medicine—for instance, the movement toward patient-centered medicine, or the backlash against the overuse of drugs and surgery that the New Yorker writer Atul Gawande calls “the epidemic of unnecessary care.”
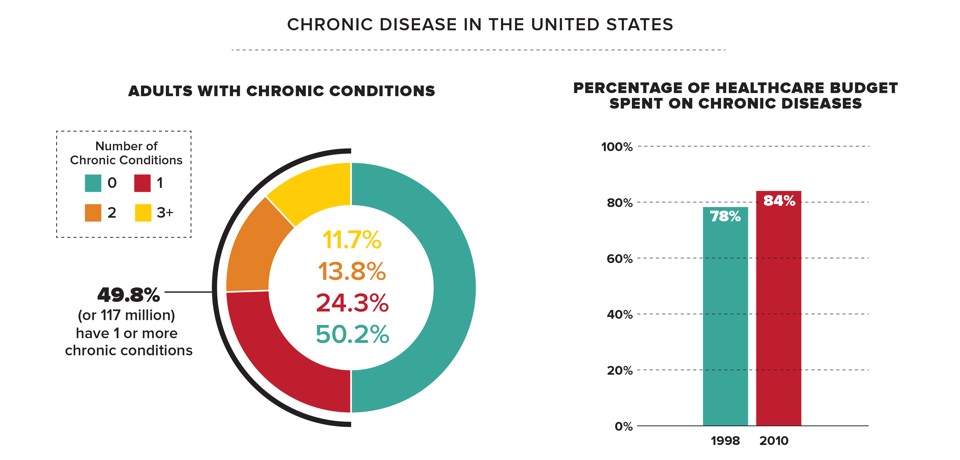
When Blackwelder teaches family medicine at East Tennessee University, he says he reminds his students to stay open to treatments that once seemed esoteric, as long as they show some promise. “A common homily we tell our students is that in five years, half of what we taught them will be wrong. We just don’t know which half,” he says. “We find things out by remaining inquisitive, being open to exploring new ideas when a question is asked. We should never just say we’ve got it all figured out, because we rarely do.”At a time when one in two American adults has at least one chronic disease, it’s safe to say there are a lot of things medicine still hasn’t figured out.
