To take the antiviral Paxlovid or not is a big question among many older adults. The drug is meant to be taken soon after a person develops a Covid-19 symptoms - to avoid severe Covid symptoms and prevent hospitalization and death. Unfortunately, some people develop rebound Covid after stopping Paxlovid - that is, they again develop Covid-19.
What is going on? How frequently does this occur? A new study recently published found a rebound effect of 21%. That's 1 in 5 persons taking Paxlovid (nirmatrelvir-ritonavir). Also, the researchers found that during the second bout with Covid the person is shedding viral particles - thus contagious, even if they didn't have symptoms during the rebound.
In comparison, the Covid rebound rate was 1.8% in persons who did not receive Paxlovid.
And yes, the rebound Paxlovid group was vaccinated. The Paxlovid group had received an average 4 vaccines vs 3 in the no treatment group. Interestingly, Covid rebound was more common among those who started Paxlovid therapy within the first 2 days of Covid symptoms, versus those who started later.
So...it's still unclear to many older adults whether to take Paxlovid or not.
From Science Daily: One in five patients experience rebound COVID after taking Paxlovid, new study finds
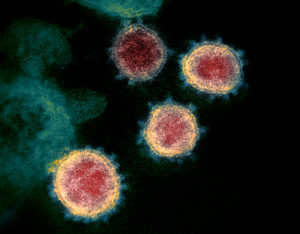
A new study by investigators from Mass General Brigham found that one in five individuals taking Nirmatrelvir-ritonavir therapy, commonly known as Paxlovid, to treat severe symptoms of COVID-19, experienced a positive test result and shedding of live and potentially contagious virus following an initial recovery and negative test -- a phenomenon known as virologic rebound.
By contrast, people not taking Paxlovid only experienced rebound about 2 percent of the time.
"We conducted this study to address lingering questions about Paxlovid and virologic rebound in COVID-19 treatment," said corresponding author Mark Siedner, M.D., MPH, an infectious disease clinician and researcher in the Division of Infectious Diseases at Massachusetts General Hospital. "We found that the virologic rebound phenomenon was much more common than expected -- in over 20% of people taking Paxlovid -- and that individuals shed live virus when experiencing a rebound, implying the potential for transmission after initially recovering from the virus."
Paxlovid is an oral antiviral medication used to treat COVID-19. Previous studies demonstrate the medication's effectiveness in reducing hospitalization and death in cases of severe COVID-19 infection. Since the integration of Paxlovid into COVID-19 treatment, some patients have reported virologic rebound. A previously conducted phase 3 clinical trial known as EPIC-HR suggested that only 1% to 2% of patients taking Paxlovid experienced virologic rebound. However, the study by Siedner and colleagues suggests this phenomenon occurs far more often than previously suspected.
"Paxlovid remains a life-saving drug I prescribe to high-risk patients," said co-senior author Jonathon Li, M.D., an infectious disease physician and researcher in the Division of Infectious Diseases at Brigham and Women's Hospital. "This study, while informative, does not change the fact that this drug is very effective at preventing hospitalizations and death. Instead, it offers valuable insights to Paxlovid patients, helping them understand what to expect and how long they might be contagious."
Siedner, Li and other researchers from Mass General Brigham collected data from the Post-vaccination Viral Characteristics Study (POSITIVES), an ongoing study following individuals diagnosed with acute COVID-19 infections. Between March 2022 and May 2023, 142 individuals were selected for the study based on positive COVID-19 tests, medication prescriptions or physician referrals. Sorting participants by those who took a five-day Paxlovid regimen versus those who did not, they closely tracked patients' viral loads and symptoms, cultured viral samples and performed whole genome sequencing. Patients who tested positive for COVID-19 after previously testing negative and those who exhibited two consecutive increases in viral loads following an initial reduction were classified as experiencing virologic rebound.
Investigators discovered that 20.8% of participants who took Paxlovid experienced virologic rebound, while only 1.8% of those who didn't take Paxlovid had a similar rebound effect. Those with rebound also had prolonged viral shedding -- for an average of 14 days compared to less than 5 days in those who did not experience rebound -- indicating they were potentially still contagious for much longer. Importantly, Siedner's team found no evidence of drug resistance among these patients.
The findings should not discourage clinicians from prescribing the medication, the researchers noted, but they should prompt them to counsel patients who take the medication about the risk for viral rebound and spreading the virus to others. Advising patients to re-test and isolate in case of rebound should be part of that conversation, the team said.
"In our study, we were able to closely monitor patients from the onset of COVID-19 infection through treatment and rebound," explained Li. "Unlike in the EPIC-HR study, which only assessed outcomes at two time points, we followed up with patients three times a week, sometimes for months, and performed in-home sample collection. Having both viral RNA levels and viral culture data also allowed us to paint a more comprehensive and nuanced picture of a patient's experience with Paxlovid."
This study is limited in that it was observational and not a randomized controlled trial, so the authors cannot be certain that the increased rebound rate seen in people taking Paxlovid was solely due to use of the drug. The team used a positive viral culture as a marker for one's risk of transmitting the virus but could not formally measure how contagious someone experiencing virologic rebound was. Additionally, the team could not explain why some people experienced rebound while others did not -- something they aim to explore with future studies. They also plan to investigate the biological mechanism behind the rebound phenomenon associated with Paxlovid and determine if changing the regimen length could help combat this rebound effect.
