
A recent study confirmed that in the skin condition called rosacea, the skin microbiome is out of whack (dysbiosis). Of course. The study also confirmed that treatment with a topical ivermectin cream helps with the inflamed red skin rashes on the face and lowers the number of Demodex mites found on the skin.
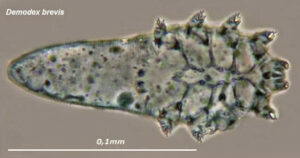
But while the cream improved symptoms in 44% of the patients, it didn't correct the skin dysbiosis. In rosacea, there is a big increase of Demodex mites (compared to normal levels) at the site of the red rashes or lesions. After the topical ivermectin cream treatment, the number of mites decreased in 88% of the rosacea group to more normal levels. [Yes, we all have Demodex mites living on our skin.]
However, other bacterial species are still different in the rosacea group compared to healthy persons without rosacea. The researchers found Cutibacterium species are predominant in healthy persons without rosacea, but are not found in persons when they have rosacea inflammation. Instead Staphylococcus species take over (just like in atopic dermatitis).
The skin microbiome is the community of bacteria, viruses, fungi that live on our skin. Rosacea is an inflammatory skin condition that typically affects the face resulting in redness, pimples, swelling, and dilated blood vessels. It frequently begins with flushing (redness) of the face in symmetrical patches, and it may or may not progress.
Excerpts from the medical site Medscape: Topical Ivermectin Study Sheds Light on Dysbiosis in Rosacea
Topical ivermectin has significant clinical efficacy and decreases the density of Demodex mites found in the skin of people with rosacea, but cutaneous dysbiosis remains, according to a report presented at the recent European Academy of Dermatology and Venereology (EADV) 2023 Congress.
"This is the first hint that the host's cutaneous microbiome plays a secondary role in the immunopathogenesis of rosacea," said Bernard Homey, MD, director of the Department of Dermatology at University Hospital Düsseldorf in Germany.
"In rosacea, we are well aware of trigger factors such as stress, UV light, heat, cold, food, and alcohol," he said. "We are also well aware that there is an increase in Demodex mites in the pilosebaceous unit."
Ivermectin Helps, but How?
Ivermectin 1% cream (Soolantra) has been approved by the US Food and Drug Administration since 2014 for the treatment of the inflammatory lesions that are characteristic of rosacea, but its mechanism of action is not clear.
The mean age of the patients with rosacea was 54.9 years, and the mean Demodex counts before and after treatment were a respective 7.2 cm2 and 0.9 cm2.
Using the Investigator's General Assessment to assess the severity of rosacea, Homey reported that 43.9% of patients with rosacea had a decrease in scores at day 30, indicating improvement.
In addition, topical ivermectin resulted in a marked or total decrease in Demodex mite density for 87.5% of patients (n = 24) who were identified as having the mites.
As a form of quality control, skin microbiome changes among the patients were compared with control patients using 16S rRNA sequencing. "The taxa we find within the cutaneous niche of inflammatory lesions of rosacea patients are significantly different from healthy volunteers," Homey said.
Cutibacterium species are predominant in healthy control persons but are not present when there is inflammation in patients with rosacea. Instead, Staphylococcus spp "take over the niche, similar to atopic dermatitis," he noted.
Looking at how treatment with ivermectin influences the organisms, the decrease in C acnes seen in patients with rosacea persisted despite treatment, and the abundance of S epidermidis, S hominis, and S capitis increased further. This suggests a possible protective or homeostatic role of C acnes but a pathogenic role for Staphylococci, explained Homey.
Homey and associates conclude in their abstract that the findings "support that rosacea lesions are associated with dysbiosis."
