 This study found impressive results - improvement in autistic behaviors in children diagnosed with autism spectrum disorder (ASD) with four months of daily vitamin D supplementation. Children in the placebo group did not show improvement. A nice aspect of the study was that the children were randomly assigned to a placebo or a vitamin D group (so that the groups were not self-selected) and it was double-blinded (so no one knew who was getting the vitamins - again to prevent bias). This was a preliminary study - meaning more studies are needed, but it would be amazing if these results hold up... From Science Daily:
This study found impressive results - improvement in autistic behaviors in children diagnosed with autism spectrum disorder (ASD) with four months of daily vitamin D supplementation. Children in the placebo group did not show improvement. A nice aspect of the study was that the children were randomly assigned to a placebo or a vitamin D group (so that the groups were not self-selected) and it was double-blinded (so no one knew who was getting the vitamins - again to prevent bias). This was a preliminary study - meaning more studies are needed, but it would be amazing if these results hold up... From Science Daily:
Vitamin D supplements may benefit children with autism spectrum disorder
Studies have shown an association between the risk of autism spectrum disorder and vitamin D insufficiency. In this latest study, 109 children with autism spectrum disorder were randomized to receive four months of vitamin D3 supplementation or a placebo."Autism symptoms -- such as hyperactivity, social withdrawal, and others -- improved significantly following vitamin D3 supplementation but not after receiving placebo," said Dr. Khaled Saad, lead author of the Journal of Child Psychology and Psychiatry study.
Excerpts from the original study from The Journal of Child Psychology and Psychiatry: Randomized controlled trial of vitamin D supplementation in children with autism spectrum disorder
Autism spectrum disorder (ASD) is a frequent developmental disorder characterized by pervasive deficits in social interaction, impairment in verbal and nonverbal communication, and stereotyped patterns of interests and activities. It has been previously reported that there is vitamin D deficiency in autistic children; however, there is a lack of randomized controlled trials of vitamin D supplementation in ASD children.
Recently, Wang et al. (2016) performed a systematic review and meta-analysis of all studies on serum concentration of 25 (OH)D in ASD (Wang et al., 2016). Eleven studies were included, accounting for a total of 870 ASD patients and 782 healthy controls. Serum levels of 25 (OH)D in participants with ASD were significantly lower than those in controls. They concluded that low vitamin D might serve as a risk factor for autism spectrum disorder (Wang et al., 2016).
In a recent survey, our research group measured 25 (OH)D in 122 ASD children (3–9 years old) and 100 healthy children as controls (Saad, Abdel-Rahman, et al., 2015). The ASD group showed a significantly lower level of serum 25 (OH)D compared with the control group (p < .0001). The study found highly significant inverse correlations between serum 25 (OH)D levels and autism rating scales. In the second part of the previous study (Saad, AbdelRahman, et al., 2015), an open-label trial of 83 subjects who completed a 3-month therapy with high daily doses of vitamin D (300 IU/kg/day) was performed. Collectively, 80.7% of the children with ASD had significantly improved outcome, which was mainly in the sections of the CARS and ABC subscales that measure behavior, stereotypy, eye contact, and attention span (Saad, Abdel-Rahman, et al., 2015).

 Guidelines for how to prevent food allergies in children are changing. Until very recently, it was avoid, avoid, avoid exposing babies or young children to any potential allergens. Remember parents being advised that if an allergy to X (whether pets or food) runs in the family, then absolutely avoid exposing the child to the potential allergen? Well, recent research (
Guidelines for how to prevent food allergies in children are changing. Until very recently, it was avoid, avoid, avoid exposing babies or young children to any potential allergens. Remember parents being advised that if an allergy to X (whether pets or food) runs in the family, then absolutely avoid exposing the child to the potential allergen? Well, recent research ( Study after study finds negative health effects from air pollution, such as heart disease (
Study after study finds negative health effects from air pollution, such as heart disease ( Uh oh - once again a drug taken for a common problem (heartburn) is linked to an unexpected negative health effect (higher risk of strokes). Millions of Americans take proton pump inhibitors (PPIs) to treat acid reflux and heartburn. They are among the most prescribed drugs in the United States, are frequently taken for long periods of time, and are available over the counter. But according to preliminary research presented at a 2016 American Heart Association conference, these medications may also increase the risk of ischemic stroke. Ischemic strokes, which are the most common type of stroke, occur when a blood clot cuts off blood flow to the brain.
Uh oh - once again a drug taken for a common problem (heartburn) is linked to an unexpected negative health effect (higher risk of strokes). Millions of Americans take proton pump inhibitors (PPIs) to treat acid reflux and heartburn. They are among the most prescribed drugs in the United States, are frequently taken for long periods of time, and are available over the counter. But according to preliminary research presented at a 2016 American Heart Association conference, these medications may also increase the risk of ischemic stroke. Ischemic strokes, which are the most common type of stroke, occur when a blood clot cuts off blood flow to the brain. An article points out what we should all be concerned with, but is being ignored - pesticide residues of glyphosate (found in Monsanto's Roundup) and 2,4-D in foods. Glyphosate is the most used pesticide in the world, and both glyphosate and 2,4-D pesticide residues in food are set to really increase with the introduction of
An article points out what we should all be concerned with, but is being ignored - pesticide residues of glyphosate (found in Monsanto's Roundup) and 2,4-D in foods. Glyphosate is the most used pesticide in the world, and both glyphosate and 2,4-D pesticide residues in food are set to really increase with the introduction of 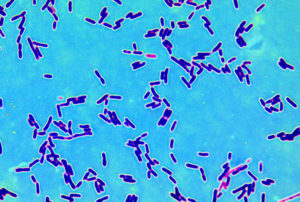 Interesting preliminary research that suggests that daily intake for 12 weeks of several beneficial bacteria species (Lactobacillus acidophilus, L. casei, L. fermentum, and Bifidobacterium bifidum) resulted in improved mental (cognitive) functioning in 52 people with Alzheimer's Disease. Could this be true - daily probiotics to improve mental functioning in those with Alzheimer's?
Interesting preliminary research that suggests that daily intake for 12 weeks of several beneficial bacteria species (Lactobacillus acidophilus, L. casei, L. fermentum, and Bifidobacterium bifidum) resulted in improved mental (cognitive) functioning in 52 people with Alzheimer's Disease. Could this be true - daily probiotics to improve mental functioning in those with Alzheimer's? The CDC (Centers for Disease Control and Prevention) released a report this week stating that tobacco use is the most preventable cause of cancer, and that 40% of US cancer cases are linked to its use. It is estimated that currently there are more than 36 million smokers in the US. For in depth information, go to the
The CDC (Centers for Disease Control and Prevention) released a report this week stating that tobacco use is the most preventable cause of cancer, and that 40% of US cancer cases are linked to its use. It is estimated that currently there are more than 36 million smokers in the US. For in depth information, go to the  An
An  An important study was recently published that documents that when pregnant women are exposed to potentially harmful chemicals in the environment around them (environmental pollutants), many of these chemicals also get transferred to the fetus. Many of the 59 chemicals looked for were detected in the newborn babies' umbilical cords (thus the chemicals had crossed the placenta to the fetus during the pregnancy). Some chemicals were measured in higher levels in the umbilical cord than in the mother (as measured in her blood), while only
An important study was recently published that documents that when pregnant women are exposed to potentially harmful chemicals in the environment around them (environmental pollutants), many of these chemicals also get transferred to the fetus. Many of the 59 chemicals looked for were detected in the newborn babies' umbilical cords (thus the chemicals had crossed the placenta to the fetus during the pregnancy). Some chemicals were measured in higher levels in the umbilical cord than in the mother (as measured in her blood), while only