
Finally, some good news in the treatment of Lyme disease. A recent study found that treating with 2 or 3 antibiotics at once is more effective in clearing Lyme disease bacteria than just treating with a course of one antibiotic (which is what is done now). In other words, a combination therapy is superior.
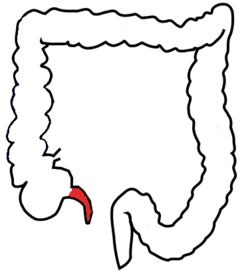
A single course of antibiotics treats most Lyme disease infections, but not in about 10 to 20% of patients. Studies find that this is because the Lyme disease bacteria hide in the organs (the sneaky devils!). The Lyme disease bacteria (Borrelia burgdorferi) is transmitted by tick bites.
 The study was done in mice with persistent Lyme disease, but the results also (probably) apply to humans with persistent Lyme disease infections. None of the single antibiotics completely eradicated the bacteria, but the following 4 dual combinations were effective: doxycycline + ceftriaxone, dapsone + rifampicin, dapsone + clofazimine, doxycycline + cefotaxime. Also effective were 3 triple antibiotic combinations: doxycycline + ceftriaxone+ carbomycin, doxycycline + cefotaxime+ loratadine, dapsone+ rifampicin+ clofazimine. The drugs were given for 28 days two months after infection.
The study was done in mice with persistent Lyme disease, but the results also (probably) apply to humans with persistent Lyme disease infections. None of the single antibiotics completely eradicated the bacteria, but the following 4 dual combinations were effective: doxycycline + ceftriaxone, dapsone + rifampicin, dapsone + clofazimine, doxycycline + cefotaxime. Also effective were 3 triple antibiotic combinations: doxycycline + ceftriaxone+ carbomycin, doxycycline + cefotaxime+ loratadine, dapsone+ rifampicin+ clofazimine. The drugs were given for 28 days two months after infection.
Next step is testing this in humans with persistent Lyme disease.
From Medical Xpress: Combined antibiotics more effective against Lyme disease: Study
Researchers at Tulane University have found that a combination of antibiotics is more effective in treating Lyme disease than the commonly prescribed course of one single antibiotic. This finding, published in Frontiers in Microbiology, could pave the way for improved Lyme disease treatments, particularly in persistent cases that have not responded to standard antibiotic treatment. ...continue reading "Combination Antibiotic Therapy May Help With Persistent Lyme Disease"

 Fermented foods include: yogurt, buttermilk, sour cream, cheese, kefir, fermented vegetables, kimchi, natto, miso, sauerkraut, traditional pickles, traditional sourdough bread, apple cider vinegar, and kombucha. To quickly improve the gut microbiome, try to eat six 1/2 cup servings each day for a
Fermented foods include: yogurt, buttermilk, sour cream, cheese, kefir, fermented vegetables, kimchi, natto, miso, sauerkraut, traditional pickles, traditional sourdough bread, apple cider vinegar, and kombucha. To quickly improve the gut microbiome, try to eat six 1/2 cup servings each day for a  Well, the following findings make total sense. A recent
Well, the following findings make total sense. A recent  The issue of
The issue of  Many people take probiotics in the belief that the probiotics will help their gut microbiome (microbial community) recover after taking antibiotics. This is because antibiotics kill both beneficial and pathogenic bacteria, and research shows it may take months for the gut to recover (it depends on the antibiotics taken). However,
Many people take probiotics in the belief that the probiotics will help their gut microbiome (microbial community) recover after taking antibiotics. This is because antibiotics kill both beneficial and pathogenic bacteria, and research shows it may take months for the gut to recover (it depends on the antibiotics taken). However,