 How does the medical profession currently view probiotics in the prevention and treatment of urinary tract infections (UTIs), especially recurrent infections? Answer: Only a few studies have been done, but what little is known is promising, which is good because traditional antibiotic treatment has problems (especially antibiotic resistance).
How does the medical profession currently view probiotics in the prevention and treatment of urinary tract infections (UTIs), especially recurrent infections? Answer: Only a few studies have been done, but what little is known is promising, which is good because traditional antibiotic treatment has problems (especially antibiotic resistance).
The following article excerpts are from Medscape. Medscape is a popular web resource for physicians and health professionals. It features peer-reviewed original medical journal articles, daily medical news, drug information, etc. To read the entire article without registering with Medscape (registration is free for everyone), just Google the title and then click on it.
From Medscape: Probiotics in Preventing Recurrent Urinary Tract Infections in Women: A Literature Review
Increasing antibiotic resistance and increasing resistance to commonly used antibiotics makes treatment and prevention of urinary tract infections difficult. Although more research is needed, probiotics should be considered a useful and safe alternative to antibiotics. Urinary tract infections (UTIs) are one of the most common bacterial infections in women, accounting for over 6 million primary care visits annually (Zak, 2014). Approximately 50% to 60% of women will develop a UTI in their lifetime...
Treatment is often complicated by the high rates of reoccurrence. Approximately 20% to 30% of women with a UTI will have a reoccurrence (Beerepoot, Geerlings, van Haarst, van Charante, & ter Riet, 2013)... Ikaheimo et al. (1996) found that in the primary care setting, 53% of women over 55 years of age and 36% of younger women will have a reoccurrence within a year. Women are diagnosed with recurrent UTIs if they have three UTIs with three positive urine cultures within a 12-month period or two infections in the previous six months (Al-Badr & Al-Shaikh, 2013).
Symptoms of UTIs include dysuria, frequency, urgency, nocturia, suprapubic pain, and hematuria, all of which significantly affect the quality of life. Contributing factors to UTIs include inadequate hydration, voiding patterns, diaphragm and spermicide use, tight undergarments, wiping technique, immuno-suppression, postmenopausal women, diabetes mellitus, and frequent sexual intercourse (Al-Badr & Al-Shaikh, 2013).
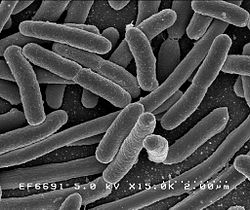
Escheria coli (E. coli) causes the majority of UTIs in women, accounting for 75% to 95% of infections (Al-Badyr & Al-Shaikh, 2013; Nosseir, Lind, & Winkler, 2012). Recurrent UTIs are most often (~80% of time) caused by reinfection with the same pathogen (Al-Badyr & Al-Shaikh, 2013; Nosseir et al., 2012).
Continuous antibiotics are currently used as treatment and prophylaxis for recurrent UTIs. The literature recommends treating anywhere from 6 to 12 months to 2 to 5 years (Zak, 2014). However, the long-term effects of antibiotics are unknown. We are currently in an age of increasing antibiotic resistance, and increasing resistance to commonly used antibiotics, such as trimethoprim-sulfamethoxazole (Gupta, Hooton, & Stamm, 2001), makes treatment and prevention of infections difficult. Therefore, finding safe and effective alternatives to preventing recurrent UTIs in women is imperative.
The literature provides low-to-moderate evidence that probiotics are effective in preventing UTIs in women. Abdulwahab, Abdulazim, Nada, and Radi (2013) examined the effect of vaginal Lactobacillus from 100 healthy women on the growth of uropathogenic E. coli isolates from 100 women with recurrent UTIs. They found that the majority of Lactobacilli in healthy women without UTIs were L. acidophilus, L. fermentum, and L. delburekii. In addition, they found that all vaginal Lactobacilli strains (from asymptomatic women) could inhibit the growth of E. coli on the agar plate. The weakness of this study, however, is that it was done in a laboratory.
Two studies went one step further by examining human prophylaxis with Lactobacilli, either orally or vaginally, as means to prevent recurrent UTIs. Beerepoot et al. (2012) compared the effects of oral L. rhamnosus and L. reuteri (109 CFU twice daily) with trimethoprim-sulfamethoxazole (TMP-SMX, 480 mg daily) on preventing recurrent UTIs in 252 postmenopausal women. In their randomized control trial, they found that after 12 months of prophylaxis, the mean number of symptomatic UTIs decreased form 7.0 (from the previous year) to 2.9 in the TMP-SMX group and from 6.8 to 3.3 in the Lactobacilli group.
Antibiotic resistance from E. coli (causing UTI and in urine and feces of asymptomatic women) to sulfamethoxazole, trimethoprim and amoxicillin increased...after 12 months of TMP-SMX prophylaxis, 100% of urinary E. coli was found resistant to trimethoprim and sulfamethoxazole. No antibiotic resistance occurred in the Lactobacilli group.
Stapleton et al. (2011) considered the effect of an intravaginal probiotic, L. crispatus, for prevention of recurrent UTIs in 100 premenopausal women. In their randomized, placebo-controlled phase 2 trial, they found that L. crispatus was associated with reduced symptomatic UTIs. Fifteen percent of women taking L. crispatus and 27% of women taking placebo experienced recurrent UTIs.
Each of the three studies above examined different species of Lactobacilli. Abdulwahab et al. (2013) investigated the effects of L. acidophilus, L. fermentum, and L. delburekii. Beerepoot et al. (2012) studied L. rhamnosus and L. reuteri and Stapleton et al. (2011) investigated L. crispatus....However, all three studies provide evidence that even with different strains of Lactobacilli and different routes of receiving the probiotic, Lactobacilli can reduce recurrent UTIs in women.
The literature review reveals that Lactobacillus probiotics, taken either orally or vaginally, are likely effective in reducing recurrent UTIs in women. Lactobacilli may be especially useful for women with a history of recurrent, complicated UTIs or prolonged antibiotic use. Although Lactobacilli are found slightly less effective to antibiotics in reducing recurrent UTIs (at least in the dose and frequency studied), probiotics do not cause antibiotic resistance and may offer other health benefits due to vaginal re-colonization with Lactobacilli. In addition, long-term health effects of continual antibiotic use are still lacking.
 E. coli bacteria. Credit: Wikipedia.
E. coli bacteria. Credit: Wikipedia.

I am antibiotic resistant with the only oral antibiotic Ampicillin other then that I need IV antibiotic
I was hospitalized 4 yrs ago with Sepsis from UTI that advanced to kidneys
Now I am looking for which Probiotic and what dose I can take to prevent or keep my gut healthy
I avoid antibiotics but developed a UTI after taking antibiotics for dental work and developing a UTI from the diarrhea caused by the antibiotic.
Any suggestions?
The use of probiotics for UTIs is still in its infancy, but it seems that Lactobacillus bacteria are beneficial. The study mentioned the following as possible good candidates: L. acidophilus, L. fermentum, and L. delburekii. L. rhamnosus, L. reuteri, and L. crispatus. One possibility is taking a probiotic daily with at least some of these species and see if this helps. I would look for one that has to be refrigerated (to increase the odds of the bacteria being alive) such as Ultimate Probiotic 12/12 Formula by Natural Factors (this one has 3 of the mentioned Lactobacillus species)..
An effective alternative treatment for UTIs (even antibiotic resistant infections) is D-mannose - which can be taken as a pill or powder (see May 18, 2015 post). Up to 95% of UTIs are caused by E.coli, and D-mannose is effective against that bacteria (as well as some others). It is a non-prescription that can be purchased online and in many stores such as Whole Foods. D-mannose is a naturally occurring sugar found in a number of fruits, especially cranberries and blueberries. One study found that D-mannose worked better than an antibiotic for preventing recurrences. See the post for details.
The literature on cranberry juice is mixed, but one can drink some cranberry juice daily or take (organic) cranberry supplements in tablet form (some people advise taking several tablets daily whenever they feel an UTI coming on).
And last, some very interesting research (see June 26, 2015 post) suggests that raising the urinary pH may prevent or treat UTIs (raising the pH may prevent bacterial growth in the urinary tract). Some dietary ways to increase pH (to make it less acidic) include drinking coffee, tea, colorful berries, red wine, and cranberries. The researchers also mention the possibility of oral bicarbonate therapy (the antacid sodium bicarbonate or baking soda) to raise the urinary pH.