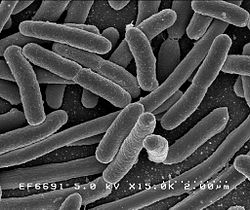
 A few days ago the CDC (Centers for Disease Control and Prevention) released a report about a Nevada woman who died in August 2016 of a bacterial infection that was resistant to all 26 antibiotics available in the US, including the antibiotic of last resort - colistin. Apparently she had picked up the bacterial infection in India, where she been staying for an extended visit and where she had been hospitalized (a fractured leg, which led to a hip infection). Because of the antibiotic resistance, the infection spread, and she went into septic shock and died.
A few days ago the CDC (Centers for Disease Control and Prevention) released a report about a Nevada woman who died in August 2016 of a bacterial infection that was resistant to all 26 antibiotics available in the US, including the antibiotic of last resort - colistin. Apparently she had picked up the bacterial infection in India, where she been staying for an extended visit and where she had been hospitalized (a fractured leg, which led to a hip infection). Because of the antibiotic resistance, the infection spread, and she went into septic shock and died.
India has soaring rates of antibiotic resistance due to misuse of antibiotics (or antimicrobials). But this is not just a problem with infections acquired in India, but throughout the world. Antibiotic resistance is increasing everywhere (post with video of how superbugs evolve). This is because bacteria are constantly evolving against the antibiotics they're exposed to. We may reach a point where simple cuts or infections could lead to death because no antibiotics will work. The World Health Organization said in a 2014 report that: "The problem is so serious that it threatens the achievements of modern medicine. A post-antibiotic era—in which common infections and minor injuries can kill—far from being an apocalyptic fantasy, is instead a very real possibility for the twenty-first century."
New antibiotic development is not keeping pace with the emergence of new antibiotic resistant bacteria. According to the CDC: "Each year in the United States, at least 2 million people become infected with bacteria that are resistant to antibiotics and at least 23,000 people die each year as a direct result of these infections." On top of that, too few antibiotics are under development, and those antibiotics tend to be developed by small companies, not the big pharmaceutical companies. Farmers are still giving antibiotics (antimicrobials) to farm animals unnecessarily, typically as "growth promoters" or to try to prevent disease. The sale of antibiotics routinely fed to animals has been increasing in recent years, and currently about 80% of all antibiotics used in the US are given to livestock animals (of which nearly 70 percent of those used are considered “medically important” for humans).
Excerpts from The Atlantic: A Woman Was Killed by a Superbug Resistant to All 26 American Antibiotics
Yesterday morning, I published a story about the silent spread of resistance against the antibiotic of last resort, colistin—a major step toward the emergence of a superbug resistant to all antibiotics. While reporting this story, I interviewed Alex Kallen, an epidemiologist at the CDC, and I asked if anyone had found such a superbug yet. “Funny you should ask,” he said.
Funny—by which we all mean scary—because yesterday afternoon, the CDC also released a report about a Nevada woman who died after an infection resistant to 26 antibiotics, which is to say all available antibiotics in the U.S. The woman, who was in her 70s, had been previously hospitalized in India after fracturing her leg, eventually which led to an infection in her hip. There was nothing to treat her infection—not colistin, not other last-line antibiotics. Scientists later tested the bacteria that killed her, and found it was somewhat susceptible to fosfomycin, but that antibiotic is not approved in the U.S. to treat her type of infection.
