 Earlier posts discussed research that showed that farm and animal (pets such as dogs) exposures in the first year of life is protective against allergies and asthma (lowers the risk of developing them). New research examined this further by looking at Amish and Hutterite groups - looking at not just "farm life", but whether children had much exposure to farm animals. The Amish have close exposure to farm animals (traditional farming methods), but the Hutterites don't (communal highly industrialized farming). Both groups studied had similar lifestyles (drank raw milk, breastfeeding, little exposure to smoking), but both groups did not have indoor pets ("taboos against indoor pets"). Thus farming methods were important for exposures to animals and their microbes.
Earlier posts discussed research that showed that farm and animal (pets such as dogs) exposures in the first year of life is protective against allergies and asthma (lowers the risk of developing them). New research examined this further by looking at Amish and Hutterite groups - looking at not just "farm life", but whether children had much exposure to farm animals. The Amish have close exposure to farm animals (traditional farming methods), but the Hutterites don't (communal highly industrialized farming). Both groups studied had similar lifestyles (drank raw milk, breastfeeding, little exposure to smoking), but both groups did not have indoor pets ("taboos against indoor pets"). Thus farming methods were important for exposures to animals and their microbes.
The researchers said: "The importance of environmental exposures in the development of asthma is most exquisitely illustrated by epidemiologic studies conducted in Central Europe that show significant protection from asthma and allergic disease in children raised on traditional dairy farms. In particular, children’s contact with farm animals and the associated high microbial exposures4,5have been related to the reduced risk." Traditional farming exposed the children to an environment rich in microbes, and these children had very low rates of asthma and "distinct immune profiles that suggest profound effects on innate immunity." Once again, note the importance of microbes in the development of the immune system. From Science Daily:
Growing up on an Amish farm protects children against asthma by reprogramming immune cells
By probing the differences between two farming communities -- the Amish of Indiana and the Hutterites of South Dakota -- an interdisciplinary team of researchers found that specific aspects of the Amish environment are associated with changes to immune cells that appear to protect children from developing asthma. In the Aug. 4, 2016, issue of The New England Journal of Medicine, the researchers showed that substances in the house dust from Amish, but not Hutterite, homes were able to engage and shape the innate immune system (the body's front-line response to most microbes) in young Amish children in ways that may suppress pathologic responses leading to allergic asthma.
The Amish and Hutterite farming communities in the United States, founded by immigrants from Central Europe in the 18th and 19th centuries, respectively, provide textbook opportunities for such comparative studies. The Amish and the Hutterites have similar genetic ancestry. They share similar lifestyles and customs, such as no television and a Germanic farming diet. They have large families, get childhood vaccinations, breastfeed their children, drink raw milk and don't allow indoor pets.
The communities, however, are distinct in two important ways. Although both groups depend on agriculture, their farming practices differ. The Amish have retained traditional methods. They live on single-family dairy farms and rely on horses for fieldwork and transportation. In contrast, the Hutterites live on large communal farms. They use modern, industrialized farm machinery. This distances young Hutterite children from the constant daily exposure to farm animals. The other striking difference is what Ober calls a "whopping disparity in asthma." About 5 percent of Amish schoolchildren aged 6 to 14 have asthma. This is about half of the U.S. average (10.3%) for children aged 5 to 14, and one-fourth of the prevalence (21.3%) among Hutterite children.
To understand this disparity, the researchers studied 30 Amish children 7 to 14 years old, and 30 age-matched Hutterite children. They scrutinized the children's genetic profiles, which confirmed the remarkable similarities between Amish and Hutterite children. They compared the types of immune cells in the children's blood, collected airborne dust from Amish and Hutterite homes and measured the microbial load in homes in both communities.
The first gee-whiz moment came from the blood studies. These revealed startling differences between the innate immune response from the Amish and Hutterites. "The Amish had more and younger neutrophils, blood cells crucial to fight infections, and fewer eosinophils, blood cells that promote allergic inflammation," said study co-author, immunologist Anne Sperling, PhD, associate professor of medicine at the University of Chicago. Gene expression profiles in blood cells also revealed enhanced activation of key innate immunity genes in Amish children.
The second eureka moment came from experiments using mice. When study co-author, immunologist Donata Vercelli, MD, professor of cellular and molecular medicine and associate director of the Asthma and Airway Disease Research Center at the University of Arizona, exposed mice to house-dust extracts, she found the airways of mice that received Amish dust were protected from asthma-like responses to allergens. In contrast, mice exposed to Hutterite house dust were not protected.
What was different? Dust collected from Amish homes was "much richer in microbial products," the authors note, than dust from Hutterite homes. "Neither the Amish nor the Hutterites have dirty homes," Ober explained. "Both are tidy. The Amish barns, however, are much closer to their homes. Their children run in and out of them, often barefoot, all day long. There's no obvious dirt in the Amish homes, no lapse of cleanliness. It's just in the air, and in the dust."
To better understand how asthma protection was achieved, the researchers used mice that lack MyD88 and Trif, genes crucial for innate immune responses. In these mice, the protective effect of the Amish dust was completely lost. "The results of the mouse experiments conclusively prove that products from the Amish environment are sufficient to confer protection from asthma, and highlight the novel, central role that innate immunity plays in directing this process," Vercelli said.

 The
The  Get active, really active, to reduce your risk for 5 diseases: breast cancer, colon cancer, heart disease, and ischemic stroke. Instead of the 150 minutes of brisk walking or 75 minutes per week of running (which is equal to the 600 metabolic equivalent (MET) minutes now recommended by the World Health Organization), this study found that much more exercise is needed for
Get active, really active, to reduce your risk for 5 diseases: breast cancer, colon cancer, heart disease, and ischemic stroke. Instead of the 150 minutes of brisk walking or 75 minutes per week of running (which is equal to the 600 metabolic equivalent (MET) minutes now recommended by the World Health Organization), this study found that much more exercise is needed for 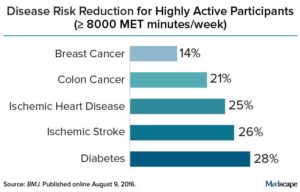 Credit: Medscape
Credit: Medscape Take note: what is happening to dogs is also happening to men. Specifically, for many decades - year by year - there has been a decrease in male dog fertility. And yes, this is also happening with human male fertility - a decline in male semen quality (including sperm), along with an increase in the incidence of testicular cancer, the birth defect hypospadias, and undescended testes. This cluster of problems is called testicular dysgenesis syndrome (TGS
Take note: what is happening to dogs is also happening to men. Specifically, for many decades - year by year - there has been a decrease in male dog fertility. And yes, this is also happening with human male fertility - a decline in male semen quality (including sperm), along with an increase in the incidence of testicular cancer, the birth defect hypospadias, and undescended testes. This cluster of problems is called testicular dysgenesis syndrome (TGS Another study reporting health benefits of drinking tart cherry juice, specifically in speeding recovery following prolonged, repeat sprint activity (think soccer and rugby). The researchers found that after a prolonged, intermittent sprint activity, the cherry juice significantly lowered levels of Interleukin-6, a marker for inflammation and that there was a decrease in muscle soreness. The study participants drank the cherry juice (1 oz cherry juice concentrate mixed with 100 ml water) for several days before and several days after the sprint activity. Montmorency tart cherry juice is a
Another study reporting health benefits of drinking tart cherry juice, specifically in speeding recovery following prolonged, repeat sprint activity (think soccer and rugby). The researchers found that after a prolonged, intermittent sprint activity, the cherry juice significantly lowered levels of Interleukin-6, a marker for inflammation and that there was a decrease in muscle soreness. The study participants drank the cherry juice (1 oz cherry juice concentrate mixed with 100 ml water) for several days before and several days after the sprint activity. Montmorency tart cherry juice is a  A recent study compared saline nasal irrigation vs steam inhalation vs doing both saline irrigation and steam inhalation vs doing neither (the control group) for chronic or recurring sinusitis symptoms. In the study, people with a history of chronic or recurring sinusitis symptoms were randomly assigned to one of the 4 groups, and then studied 3 months and 6 months later. The results were: a modest (slight improvement) in the saline irrigation group in symptom and quality-of-life scores, but no improvement for the steam inhalation group. However, the researchers noted that the control group also had slight improvements at 3 and 6 months. Most of the improvement in the saline irrigation group was in the group that also did steam inhalation - thus perhaps some benefit to combining both.
A recent study compared saline nasal irrigation vs steam inhalation vs doing both saline irrigation and steam inhalation vs doing neither (the control group) for chronic or recurring sinusitis symptoms. In the study, people with a history of chronic or recurring sinusitis symptoms were randomly assigned to one of the 4 groups, and then studied 3 months and 6 months later. The results were: a modest (slight improvement) in the saline irrigation group in symptom and quality-of-life scores, but no improvement for the steam inhalation group. However, the researchers noted that the control group also had slight improvements at 3 and 6 months. Most of the improvement in the saline irrigation group was in the group that also did steam inhalation - thus perhaps some benefit to combining both. Another interesting study looking at whether being overweight is linked to premature death, heart attacks, and diabetes. This study looked at sets of twins, in which one is heavier than the other, and followed them long-term (average 12.4 years) and found that NO - being overweight or obese (as measured by Body Mass Index or BMI) is NOT associated with premature death or heart attack (myocardial infarction), but it is associated with higher rates of type 2 diabetes. These results are in contrast with what
Another interesting study looking at whether being overweight is linked to premature death, heart attacks, and diabetes. This study looked at sets of twins, in which one is heavier than the other, and followed them long-term (average 12.4 years) and found that NO - being overweight or obese (as measured by Body Mass Index or BMI) is NOT associated with premature death or heart attack (myocardial infarction), but it is associated with higher rates of type 2 diabetes. These results are in contrast with what