 A recent study compared saline nasal irrigation vs steam inhalation vs doing both saline irrigation and steam inhalation vs doing neither (the control group) for chronic or recurring sinusitis symptoms. In the study, people with a history of chronic or recurring sinusitis symptoms were randomly assigned to one of the 4 groups, and then studied 3 months and 6 months later. The results were: a modest (slight improvement) in the saline irrigation group in symptom and quality-of-life scores, but no improvement for the steam inhalation group. However, the researchers noted that the control group also had slight improvements at 3 and 6 months. Most of the improvement in the saline irrigation group was in the group that also did steam inhalation - thus perhaps some benefit to combining both.
A recent study compared saline nasal irrigation vs steam inhalation vs doing both saline irrigation and steam inhalation vs doing neither (the control group) for chronic or recurring sinusitis symptoms. In the study, people with a history of chronic or recurring sinusitis symptoms were randomly assigned to one of the 4 groups, and then studied 3 months and 6 months later. The results were: a modest (slight improvement) in the saline irrigation group in symptom and quality-of-life scores, but no improvement for the steam inhalation group. However, the researchers noted that the control group also had slight improvements at 3 and 6 months. Most of the improvement in the saline irrigation group was in the group that also did steam inhalation - thus perhaps some benefit to combining both.
In addition, patients in the nasal irrigation group reported fewer headaches, fewer of them used over-the-counter medications, and said they were less likely to consult with a physician about their nasal problems in the future when compared with patients in the steam inhalation group.
Most people with chronic or recurring sinusitis will probably agree with the findings. Yes, effects are modest with saline irrigation, but it definitely does improve nasal stuffiness (experiences of family members and readers). But it does NOT treat the sinusitis. The sinus microbial community continues to stay out of whack (dysbiosis). Which explains the researchers' finding that saline irrigation and steam inhalation did not result in differences in antibiotic use or physician visits after 6 months.
From Science Daily: Nasal irrigation may prevent chronic sinus ailments
Advising patient with chronic sinus congestion to use nasal irrigation -- a popular nonpharmacologic treatment -- improved their symptoms, but steam inhalation did not, according to a randomized controlled trial published in CMAJ(Canadian Medical Association Journal). More than 25 million people in the United States and about 2.5 million Canadians suffer from chronic rhinosinusitis, or sinus infection, and experience compromised quality of life. To alleviate symptoms, steam inhalation and nasal irrigation are widely suggested as an alternative to common treatment with antibiotics, which are often not effective and contribute to antibiotic resistance.
Researchers from the United Kingdom conducted a randomized controlled trial on the effectiveness of advice from primary care physicians to use nasal irrigation and/or steam inhalation for chronic sinusitis. The study involved 871 patients from 72 primary care practices in England who were randomly assigned to 1 of 4 advice strategies: usual care, daily nasal and saline irrigation supported by a demonstration video, daily steam inhalation, or combined treatment with both interventions.
Patients who were instructed to use nasal irrigation showed improvement at 3 and 6 months, as measured by the Rhinosinusitis Disability Index. Steam inhalation did not appear to alleviate symptoms of sinusitis.
"We found potentially important changes in other outcomes; in particular, fewer participants in the nasal irrigation group than in the no-irrigation group had headaches, used over-the-counter medications and intended to consult a doctor in future episodes," write the authors. "Although there was no significant difference in either physician visits or antibiotic use, as might be expected over only a 6-month follow-up period, our findings concerning consultations are important in the longer term, given antibiotic use increases the risk of antimicrobial resistance."
The Abstract (summary) of the study, which is from the Canadian Medical Association Journal (CMAJ): Effectiveness of steam inhalation and nasal irrigation for chronic or recurrent sinus symptoms in primary care: a pragmatic randomized controlled trial
ABSTRACT Background: Systematic reviews support nasal saline irrigation for chronic or recurrent sinus symptoms, but trials have been small and few in primary care settings. Steam inhalation has also been proposed, but supporting evidence is lacking. We investigated whether brief pragmatic interventions to encourage use of nasal irrigation or steam inhalation would be effective in relieving sinus symptoms.
Methods: We conducted a pragmatic randomized controlled trial involving adults (age 18–65 yr) from 72 primary care practices in the United Kingdom who had a history of chronic or recurrent sinusitis and reported a “moderate to severe” impact of sinus symptoms on their quality of life. Participants were recruited between Feb. 11, 2009, and June 30, 2014, and randomly assigned to 1 of 4 advice strategies: usual care, daily nasal saline irrigation supported by a demonstration video, daily steam inhalation, or combined treatment with both interventions. The primary outcome measure was the Rhinosinusitis Disability Index (RSDI). Patients were followed up at 3 and 6 months. We imputed missing data using multiple imputation methods.
Results: Of the 961 patients who consented, 871 returned baseline questionnaires (210 usual care, 219 nasal irrigation, 232 steam inhalation and 210 combined treatment). A total of 671 (77.0%) of the 871 participants reported RSDI scores at 3 months. Patients’ RSDI scores improved more with nasal irrigation than without nasal irrigation by 3 months (crude change −7.42 v. −5.23; estimated adjusted mean difference between groups −2.51, 95% confidence interval −4.65 to −0.37). By 6 months, significantly more patients maintained a 10-point clinically important improvement in the RSDI score with nasal irrigation (44.1% v. 36.6%); fewer used over-the-counter medications (59.4% v. 68.0%) or intended to consult a doctor in future episodes. Steam inhalation reduced headache but had no significant effect on other outcomes. The proportion of participants who had adverse effects was the same in both intervention groups.
Interpretation: Advice to use steam inhalation for chronic or recurrent sinus symptoms in primary care was not effective. A similar strategy to use nasal irrigation was less effective than prior evidence suggested, but it provided some symptomatic benefit.

 Another interesting study looking at whether being overweight is linked to premature death, heart attacks, and diabetes. This study looked at sets of twins, in which one is heavier than the other, and followed them long-term (average 12.4 years) and found that NO - being overweight or obese (as measured by Body Mass Index or BMI) is NOT associated with premature death or heart attack (myocardial infarction), but it is associated with higher rates of type 2 diabetes. These results are in contrast with what
Another interesting study looking at whether being overweight is linked to premature death, heart attacks, and diabetes. This study looked at sets of twins, in which one is heavier than the other, and followed them long-term (average 12.4 years) and found that NO - being overweight or obese (as measured by Body Mass Index or BMI) is NOT associated with premature death or heart attack (myocardial infarction), but it is associated with higher rates of type 2 diabetes. These results are in contrast with what  Studies have found that increased nut consumption has been associated with
Studies have found that increased nut consumption has been associated with  Yup, e-cigarettes are NOT harmless, but emit harmful compounds. Researchers detected significant levels of 31 chemical compounds, including nicotine, nicotyrine, formaldehyde, acetaldehyde, glycidol, acrolein, acetol, and diacetyl. Included in the harmful emissions are carcinogens and respiratory irritants. From Science Daily:
Yup, e-cigarettes are NOT harmless, but emit harmful compounds. Researchers detected significant levels of 31 chemical compounds, including nicotine, nicotyrine, formaldehyde, acetaldehyde, glycidol, acrolein, acetol, and diacetyl. Included in the harmful emissions are carcinogens and respiratory irritants. From Science Daily:
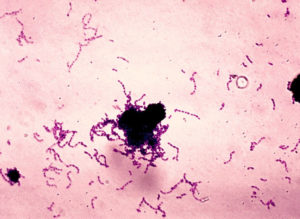 Research shows that Streptococcus mutans, the bacteria that is a main cause of tooth decay or dental caries, is passed from mother to child, and also between nonrelative children. Any interaction that involves
Research shows that Streptococcus mutans, the bacteria that is a main cause of tooth decay or dental caries, is passed from mother to child, and also between nonrelative children. Any interaction that involves  A new study followed adults with meniscus tears (in the knee), who were randomly assigned to either exercise only or meniscus repair surgery (arthroscopic partial meniscectomy) only. They found that after 2 years there was no difference between those who just received exercise therapy compared to those who just received meniscus repair surgery. About 19% of the exercise only group decided to get surgery at some point, but the rest stayed in the exercise only group.
A new study followed adults with meniscus tears (in the knee), who were randomly assigned to either exercise only or meniscus repair surgery (arthroscopic partial meniscectomy) only. They found that after 2 years there was no difference between those who just received exercise therapy compared to those who just received meniscus repair surgery. About 19% of the exercise only group decided to get surgery at some point, but the rest stayed in the exercise only group. Everyone lifting light weights during exercise workouts will be heartened by a study that found that lifting
Everyone lifting light weights during exercise workouts will be heartened by a study that found that lifting 