 Bottom line: Try to avoid artificial sweeteners!
Bottom line: Try to avoid artificial sweeteners!
From Scientific American: Artificial Sweeteners May Have Despicable Impacts on Gut Microbes
I find it ironic that Thanksgiving coincides with American Diabetes Month. In honor of that irony, two recently published studies have suggested a possible link between what you eat, how it impacts the behavior of the microbes living in your gut, and type II diabetes.
Results from a study by researchers in Israel, published in the journal Nature in October, have suggested that consumption of artificial sweeteners—found in over 6,000 food products—can lead to changes in the gut microbiome, and have put forth an explanation for how this alteration might be associated with diseases such as type II diabetes.
Jotham Suez, a PhD candidate and lead author of the study explains, “We asked people who do not regularly consume artificial sweeteners to add them to their diet for one week, and saw that the majority of these subjects had poorer glycemic responses.” And like humans, mice that were given saccharin-spiked water also developed marked glucose intolerance compared to mice drinking sugar water, or water alone.
Their experiment revealed that mice did exhibit different microbiome profiles after consuming artificial sweeteners, just as with the human volunteers who had developed glucose intolerance. And importantly, the humans who did not show glucose intolerance after consuming artificial sweeteners also did not see changes in the community composition of their microbiome.
Consequently, this change in microbial community in mice also modified how the microbiota functioned as a group to regulate metabolism. Pathways that impact the transport of sugar in the body were found to have decreased function after saccharin treatment and, notably, there was an increased abundance of short-chain fatty acids (SCFAs), which are implicated in lipid biosynthesis.
An investigation done by an independent group of researchers in Canada found similar results in a study published in October in the journal PLoS ONE. Although conducted using rats instead of mice, and with a different artificial sweetener (aspartame instead of saccharin) this study also found an increased risk of glucose intolerance. In addition, both studies showed that propionate—a SCFA highly involved in sugar production—is increased in animals consuming artificial sweeteners (although, unfortunately, propionate concentrations in humans weren’t assessed in the Nature study).
But the take home point is this: findings from two independent studies suggest that messing with the microbiome may have despicable consequences. Artificial sweeteners were originally intended to stave off the increasing obesity and metabolic disease epidemic, but instead they may have directly contributed to it.
In other words, consuming artificial sweeteners appears to throw metabolism out of whack by upsetting the critical balance of the biota in the gut—just as how chaos would surely ensue if you were to throw Gru’s minions out of whack.

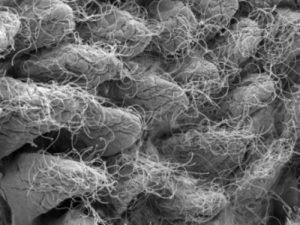 This image depicts gut microbiota.
This image depicts gut microbiota.