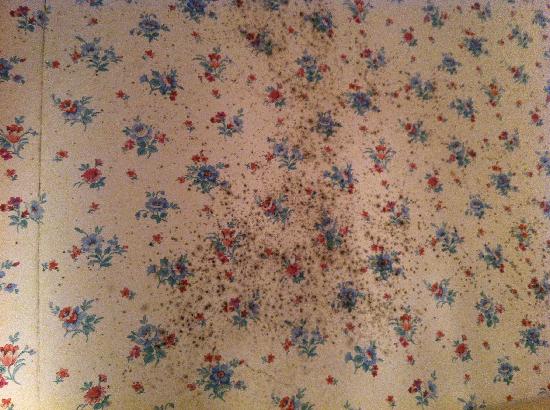
 How many people know this? That wallpaper could have fungi (mold) living on it, and this fungi can release toxins (mycotoxins) that can pollute the air and sicken people when people inhale the toxins. The releasing of toxins from the fungi (mold) into the air is called aerosolization - and when this indoor air pollution causes people living or working in the building to become sick, it is called sick building syndrome. This study looked at 3 common indoor fungal species: Penicillium brevicompactum, Aspergillus versicolor, and Stachybotrys chartarum, and the mycotoxins they produce after growing on wallpaper.
How many people know this? That wallpaper could have fungi (mold) living on it, and this fungi can release toxins (mycotoxins) that can pollute the air and sicken people when people inhale the toxins. The releasing of toxins from the fungi (mold) into the air is called aerosolization - and when this indoor air pollution causes people living or working in the building to become sick, it is called sick building syndrome. This study looked at 3 common indoor fungal species: Penicillium brevicompactum, Aspergillus versicolor, and Stachybotrys chartarum, and the mycotoxins they produce after growing on wallpaper.
Why does fungi grow on some wallpaper? The researchers write that: "Many fungi can develop on building material in indoor environments if moisture is high enough". So either high humidity in the home (especially when the weather is hot) or water damage can result in mold growth. It is estimated that in Northern Europe and North America about 20 to 40 % of buildings have visible fungal growth on surfaces. How do the mycotoxins get into the air and move around inside the home? Ordinary living, with people moving around rooms, slamming doors, air drafts from opening windows, and ceiling fans all cause "air velocities" that move around the toxins. Please note that we normally breathe in fungi and bacteria, but inhaling an overload of mycotoxins from moldy wallpaper can sicken a person. From News-Medical:
Fungal toxins from wallpaper source of illness says new research
According to a new study, there are several toxins from fungi that could be released into the air indoors and the source could be fungi living in the wall papers. These may lead to serious health problems say researchers. These ordinary fungi that live with the household wallpaper are basically of three types found the study researchers. They can grow and eventually spread to the air. This leads to serious health consequences. These effects of transmission of the airborne fungi and their toxins on human health have not been studied or considered with importance till date say researchers.
The toxins released from the fungi are called mycotoxins. They can pollute the indoor air and lead to indoor air pollution – a condition called sick building syndrome. Sick building syndrome is a condition where the residents start to feel ill according to the time they have spent in a building.... Study co-author Jean-Denis Bailly, a professor of food hygiene at the National Veterinary School of Toulouse in France in a statement explained that these mycotoxins are released from moldy material of growth of the fungi. They are eventually inhaled by the inhabitants of the home. While investigating the quality of air indoors especially at homes that have higher fungal contamination, the indoor air quality also needs to be tested for fungal toxins, he explained.
According to researchers, there has been extensive study of fungal contamination of food. However there has been little work in terms of fungal toxins in air. For this study they looked at three fungi that commonly also contaminated foods - Penicillium brevicompactum, Aspergillus versicolor and Stachybotrys chartarum. A piece of wallpaper was found to be contaminated with these three fungi. A flowing stream of air was allowed over the wallpaper and samples of air of the room were then collected for testing.
On analysis of the indoor air the researchers found that the small particles of dust floating around in the house which could then be inhaled easily, contained toxins from these fungi. Also all fungi did not spread the toxins at the same rates they found. Some spread more toxins than others and this could help researchers to decide on which fungi species to concentrate on in terms of disease prevention they said.

 Red meat allergies from a lone star tick bite? I first read about this a few years ago in
Red meat allergies from a lone star tick bite? I first read about this a few years ago in  Once again several studies found health benefits associated with drinking coffee daily - this time "reduced risk of death" in 2 studies, and in one study a reduced risk of gallbladder cancer.
Once again several studies found health benefits associated with drinking coffee daily - this time "reduced risk of death" in 2 studies, and in one study a reduced risk of gallbladder cancer. Lately more and more research has been finding health benefits with frequent consumption of extra virgin olive oil (EVOO). It is also a basic part of the popular Mediterranean diet - which emphasizes fresh fruits and vegetables, nuts, legumes (beans), whole grains, some fish, and extra virgin olive oil. Now a study conducted by investigators at Temple University in Philadelphia, Pennsylvania, suggests that the olive oil in the Mediterranean diet probably promotes healthy brain aging. The researchers said: "Our study is the first demonstration that EVOO can beneficially affect memory, amyloid plaques, and tau pathology, the hallmark lesions in the brain of Alzheimer's patients."
Lately more and more research has been finding health benefits with frequent consumption of extra virgin olive oil (EVOO). It is also a basic part of the popular Mediterranean diet - which emphasizes fresh fruits and vegetables, nuts, legumes (beans), whole grains, some fish, and extra virgin olive oil. Now a study conducted by investigators at Temple University in Philadelphia, Pennsylvania, suggests that the olive oil in the Mediterranean diet probably promotes healthy brain aging. The researchers said: "Our study is the first demonstration that EVOO can beneficially affect memory, amyloid plaques, and tau pathology, the hallmark lesions in the brain of Alzheimer's patients." The following is a study with weird results, really weird results. And it makes me think of all the times I've heard people joke: "just smelling food makes me gain weight", because we all knew it wasn't true. But what if it was true? .... The results of this study done in mice are that actually smelling the food one eats results in
The following is a study with weird results, really weird results. And it makes me think of all the times I've heard people joke: "just smelling food makes me gain weight", because we all knew it wasn't true. But what if it was true? .... The results of this study done in mice are that actually smelling the food one eats results in 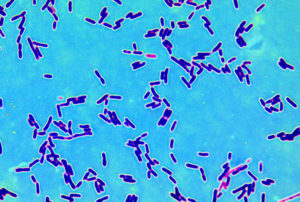 Could probiotics be used to treat depression? The medical site Medscape reported on a very small preliminary study (only 10 people) that tested that idea, with findings that suggested that taking certain probiotics does help treat the symptoms of mild to moderate depression. The bacteria taken were Lactobacillus helveticus and Bifidobacterium longum (in the product Probio'Stick). Specifically, the symptoms of mood, anhedonia (inability to feel pleasure), and sleep disturbance were significantly reduced after probiotoc therapy.
Could probiotics be used to treat depression? The medical site Medscape reported on a very small preliminary study (only 10 people) that tested that idea, with findings that suggested that taking certain probiotics does help treat the symptoms of mild to moderate depression. The bacteria taken were Lactobacillus helveticus and Bifidobacterium longum (in the product Probio'Stick). Specifically, the symptoms of mood, anhedonia (inability to feel pleasure), and sleep disturbance were significantly reduced after probiotoc therapy.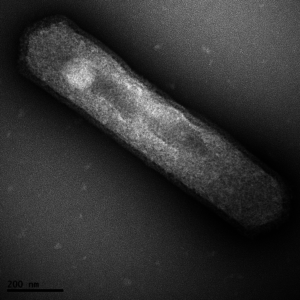 Something new to add to the list of what is in our skin microbiome - the community of microbes (bacteria, fungi, viruses) living on our skin. It turns out we also have archaea, which are
Something new to add to the list of what is in our skin microbiome - the community of microbes (bacteria, fungi, viruses) living on our skin. It turns out we also have archaea, which are  A study of 60 million Americans 65 years old and older (the entire Medicare population) found that long-term exposure to airborne fine particulate matter (PM2.5) and ozone at concentrations below current national standards increases the risk of premature death ("all cause mortality") even when the levels are below current national standards. This effect was most pronounced among racial minorities and people with low income. The national standards are called
A study of 60 million Americans 65 years old and older (the entire Medicare population) found that long-term exposure to airborne fine particulate matter (PM2.5) and ozone at concentrations below current national standards increases the risk of premature death ("all cause mortality") even when the levels are below current national standards. This effect was most pronounced among racial minorities and people with low income. The national standards are called