 More and more negative news about phthalates: men with greater exposure to DEHP (a phthalate) have lower sperm motility (how the sperm move or their ability to swim), and pregnant women with higher levels of phthalates have a higher rate of pregnancy loss (miscarriages - mainly between 5 and 13 weeks of pregnancy). Phthalates are found in many plastics, are thought to be endocrine disruptors, and can be measured in urine. From Medical Xpress: Lower sperm motility in men exposed to common chemical
More and more negative news about phthalates: men with greater exposure to DEHP (a phthalate) have lower sperm motility (how the sperm move or their ability to swim), and pregnant women with higher levels of phthalates have a higher rate of pregnancy loss (miscarriages - mainly between 5 and 13 weeks of pregnancy). Phthalates are found in many plastics, are thought to be endocrine disruptors, and can be measured in urine. From Medical Xpress: Lower sperm motility in men exposed to common chemical
Men with higher exposure to the substance DEHP, a so-called phthalate, have lower sperm motility and may therefore experience more difficulties conceiving children, according to a Lund University study. Phthalates is an umbrella term for a group of substances based on phthalic acid, some of which are suspected to be endocrine disruptors. Many phthalates are found in soft plastics in our daily surroundings.... Since phthalate molecules leak out of plastics, we are exposed to it daily and absorb the chemicals through food, drink, skin contact and inhalation.
"We have studied metabolite levels of the phthalate DEHP (diethylhexyl phthalate) in urine as an indicator of exposure, as well as the semen quality of 300 men between the ages of 18 and 20. The results show that the higher metabolite levels the men had, the lower their sperm motility was", says Jonatan Axelsson, researcher at the Department of Laboratory Medicine, Lund University. For the one quarter of the men with the lowest levels of exposure, 57 per cent of the sperm cells were moving forward, compared to 46 per cent for the quarter of the men with the highest levels of exposure.
As previous research has reported that there is a linear connection also between sperm motility and chances of becoming pregnant, the findings could indicate that the more exposed one is to DEHP, the smaller the chances are of having children.
From Medical Xpress: Exposure to phthalates could be linked to pregnancy loss
A new study of more than 300 women suggests that exposure to certain phthalates—substances commonly used in food packaging, personal-care and other everyday products—could be associated with miscarriage, mostly between 5 and 13 weeks of pregnancy.
Out of concern over the potential health effects of phthalates, the U.S. has banned six of these substances from use in certain products made for young children. But many are still included as ingredients in paints, medical tubes, vinyl flooring, soaps, shampoos and other items. Research on phthalates has shown that long-term exposure to low levels of the some of these compounds harms lab animals' health and can increase their risk for pregnancy loss. Additionally, at least one study found that female factory workers exposed to high levels of phthalates through their work were at a higher risk for miscarriage.
The researchers tested urine samples from 132 women who had miscarriages and 172 healthy pregnant women in China. They found pregnancy loss was associated with higher levels of urinary phthalate metabolites from diethyl phthalate (DEP), di-isobutyl phthalate (DiBP) and di-n-butyl phthalate (DnBP). Although this doesn't prove that phthalates cause pregnancy loss, the study suggests an association exists that the researchers say should be studied further.

 When we think about air pollution, we usually think about pollutants in the air that we breathe in. But there is a growing body of evidence that some pollutants found in the air, including a group of chemicals called phthalates, can be absorbed directly through the skin (
When we think about air pollution, we usually think about pollutants in the air that we breathe in. But there is a growing body of evidence that some pollutants found in the air, including a group of chemicals called phthalates, can be absorbed directly through the skin ( We can't see them, but we all have little face mites that live in our faces, specifically in hair follicles. The scientific name of the face mites: Demodex folliculorum. There are at least 4 lineages of face mites that correspond to different regions of the world. Good thing they're harmless (we think).Gross but fascinating. From Wired:
We can't see them, but we all have little face mites that live in our faces, specifically in hair follicles. The scientific name of the face mites: Demodex folliculorum. There are at least 4 lineages of face mites that correspond to different regions of the world. Good thing they're harmless (we think).Gross but fascinating. From Wired: So many people I know complain of carpal tunnel syndrome, especially those who spend hours every day at a computer keyboard. Carpal tunnel syndrome is a hand and arm condition of numbness, pain, tingling, etc. caused by a pinched nerve in your wrist (pressure or compression of the median nerve). Treatments vary from physical therapy to steroids to surgery, with surgery being the recommended option by many doctors. So what is best?
So many people I know complain of carpal tunnel syndrome, especially those who spend hours every day at a computer keyboard. Carpal tunnel syndrome is a hand and arm condition of numbness, pain, tingling, etc. caused by a pinched nerve in your wrist (pressure or compression of the median nerve). Treatments vary from physical therapy to steroids to surgery, with surgery being the recommended option by many doctors. So what is best?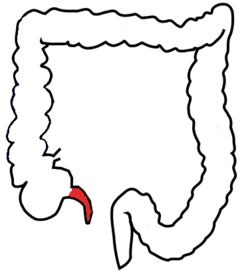
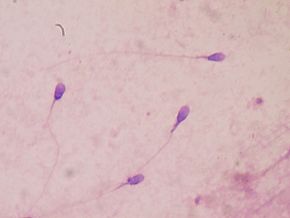 Recent research looked at environmental causes of male infertility, specifically endocrine-disrupting chemicals.
Recent research looked at environmental causes of male infertility, specifically endocrine-disrupting chemicals. It seems that a lot has been written about the health benefits of some berries, such as blueberries, while other berries have been neglected. This study focused on red raspberries, black raspberries, and blackberries. While the study was done in Poland, it was pointed out that these berries are also commonly grown in the USA. Red raspberry, black raspberry, and blackberry fruits are abundant in dietary phytochemicals such as flavonols, phenolic acids, ellagitannins, vitamins C and E, folic acid, and β-sitosterol. Many of these bioactive compounds exhibit antioxidant activity. Anthocyanins and other phenolic compounds such as ellagitannins and ellagic acid, which distinguish raspberry from other berries, occur in high levels and are mainly responsible for their broad beneficial health properties (including anti-inflammatory, antimicrobial, and antiviral activities).
It seems that a lot has been written about the health benefits of some berries, such as blueberries, while other berries have been neglected. This study focused on red raspberries, black raspberries, and blackberries. While the study was done in Poland, it was pointed out that these berries are also commonly grown in the USA. Red raspberry, black raspberry, and blackberry fruits are abundant in dietary phytochemicals such as flavonols, phenolic acids, ellagitannins, vitamins C and E, folic acid, and β-sitosterol. Many of these bioactive compounds exhibit antioxidant activity. Anthocyanins and other phenolic compounds such as ellagitannins and ellagic acid, which distinguish raspberry from other berries, occur in high levels and are mainly responsible for their broad beneficial health properties (including anti-inflammatory, antimicrobial, and antiviral activities). New research showed that eight days after a concussion, the concussed athletes (football players) looked and felt like they had recovered (clinical recovery), but MRIs showed that there were still neurophysiological abnormalities (significant blood flow decrease) in their brains. They did not look at if and when the blood flow returned to normal, but that research also needs to be done.
New research showed that eight days after a concussion, the concussed athletes (football players) looked and felt like they had recovered (clinical recovery), but MRIs showed that there were still neurophysiological abnormalities (significant blood flow decrease) in their brains. They did not look at if and when the blood flow returned to normal, but that research also needs to be done.