This is the latest study raising health concerns about energy drinks, which include popular brands Red Bull and Monster. (See review article Energy Beverages: Content and Safety and from Time What’s In Your Energy Drink? ). And remember, they are not a "real food" when you look at the ingredients (e.g., caffeine, taurine and glucuronolactone, artificial flavors, artificial sweeteners, colors). From Live Science:
Energy Drinks Raise Blood Pressure, Study Finds
Energy drinks might give you some pep — but they might also be priming you for heart problems, a new study finds. Researchers found that energy drinks can raise blood pressure to potentially unhealthy levels. The effect was far more prominent in young adults who did not consume caffeine regularly, according to the study, presented March 14 at an American College of Cardiology meeting in San Diego.
In this study, the research team — led by Dr. Anna Svatikova, a cardiovascular-diseases fellow at the Mayo Clinic in Rochester, Minnesota — gave a can of a commercially available energy drink to 25 healthy volunteers, whose ages ranged from 19 to 40. On a different day, the participants drank the same amount of a placebo drink. The researchers measured the participants' heart rate and blood pressure before and after the drinks.
The participants experienced a more marked rise in blood pressure after consuming the energy drink than after drinking the placebo, according to the findings. The participants' average systolic blood pressure (the top number in a blood pressure reading) increased by 3 percent more after they drank an energy drink, compared with after they drank the placebo drink. [5 Health Problems Linked to Energy Drinks]
The effect was most dramatic in people who did not typically consume more than a small cup of coffee or other caffeinated drink daily. In this so-called "caffeine-naive" group, the blood pressure increase was twice as high as the increase seen in the people who drank at least the equivalent of a cup of coffee on a daily basis, the researchers said in a statement...Scientists do not know whether it is the caffeine, taurine or other ingredients found in energy drinks — or a combination of ingredients — that can adversely affect the heart.
In a separate study, presented last year at an American Heart Association meeting by Maj. Emily Fletcher of the David Grant Air Force Medical Center, healthy volunteers experienced a greater increase in blood pressure after they consumed an energy drink compared to after they drank a coffee drink that had an equal amount of caffeine. This result, Fletcher said, suggests that ingredients in the energy drink other than caffeine were conspiring to raise blood pressure.

 For years there has been discussion about curcumin's anti-inflammatory, anti-bacterial, and anti-cancer effects, but more research is needed (some trials are going on now). Curcumin is a chemical compound found in turmeric. Turmeric is a member of the ginger family. It is used as a spice and is a common ingredient in Indian cooking, but also used in Middle Eastern and South Asian recipes.From Medical Xpress;
For years there has been discussion about curcumin's anti-inflammatory, anti-bacterial, and anti-cancer effects, but more research is needed (some trials are going on now). Curcumin is a chemical compound found in turmeric. Turmeric is a member of the ginger family. It is used as a spice and is a common ingredient in Indian cooking, but also used in Middle Eastern and South Asian recipes.From Medical Xpress; What was really interesting in the
What was really interesting in the  A big study that found that eating a greater proportion of plant-based foods (fruits, vegetables, grains, beans, potatoes, nuts, olive oil), as compared to animal-based foods, is linked to lower risks of dying from heart disease and stroke.
A big study that found that eating a greater proportion of plant-based foods (fruits, vegetables, grains, beans, potatoes, nuts, olive oil), as compared to animal-based foods, is linked to lower risks of dying from heart disease and stroke.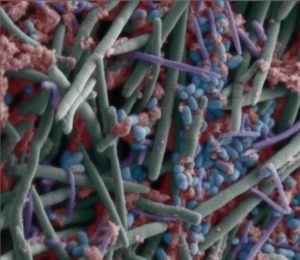 Gut bacteria in children varies among different Asian countries. A
Gut bacteria in children varies among different Asian countries. A  A
A