 Interesting idea - that perhaps our community of gut microbes being out of whack (dysbiosis) leads to hypertension. This study was done in both humans and mice - with an analysis of bacteria in both hypertensive individuals and pre-hypertensives, and also healthy individuals (the controls). Then the microbes from 2 hypertensive individuals were transplanted into mice (fecal microbiota transplants). And lo and behold - the mice became hypertensive with an alteration of their gut microbes. This is amazing!
Interesting idea - that perhaps our community of gut microbes being out of whack (dysbiosis) leads to hypertension. This study was done in both humans and mice - with an analysis of bacteria in both hypertensive individuals and pre-hypertensives, and also healthy individuals (the controls). Then the microbes from 2 hypertensive individuals were transplanted into mice (fecal microbiota transplants). And lo and behold - the mice became hypertensive with an alteration of their gut microbes. This is amazing!
The study showed that transplanting microbes from hypertensives to non-hypertensives caused an elevation in blood pressure in the formerly healthy group. This shows the direct influence of gut microbes on blood pressure. The bacteria found in both the pre-hypertensives and hypertensives (especially an overgrowth of Prevotella and Klebsiella bacteria) are those linked to inflammation. And what kind of diet is linked to that bacteria? A high fat diet. Yes, the Western diet with lots of fat and highly processed foods.
The researchers talked about other research also showing Prevotella being associated not only with hypertension, but also other diseases (e.g., periodontal diseases and rheumatoid arthritis). On the other hand, Faecalibacterium, Oscillibacter, Roseburia, Bifidobacterium, Coprococcus, and Butyrivibrio, which were "enriched" in healthy controls, were lower in pre-hypertensive and hypertensive persons. In the past I have posted about a "special" bacteria that is even called a "keystone" gut bacteria - Faecalibacterium prausnitzii - that is linked to health and is low or absent in the gut in a number of diseases ((here and here). It is not available in a supplement at this time (because it dies within a few minutes upon exposure to oxygen), but diet influences it. A high animal meat, high animal fat, high sugar, highly processed foods, and low fiber diet (the typical Western diet) lowers F. prausnitzii numbers, while a high-fiber, low meat diet increases F. prausnitzii numbers.
What you can do: Feed the beneficial gut microbes by increasing the amount of fruits, vegetables, whole grains, seeds, nuts that you eat. And cut back on the greasy, high fat processed and fast foods.
The following excerpt is misleading - for example, it ignores the first part of the actual study which looked at the gut bacteria of pre-hypertensives, hypertensive, and healthy people. Then gut bacteria from hypertensive people were transplanted into healthy mice, and gut bacteria from healthy people were transplanted into hypertensive mice. Also, it wasn't rats, but mice used in the study. It goes to show why it's important to look at original studies - not just believe articles out there blindly. [See original study.] From Science Daily: Unhealthy gut microbes a cause of hypertension, researchers find
Researchers have found that the microorganisms residing in the intestines (microbiota) play a role in the development of high blood pressure in rats mice....Scientists studied two sets of rats mice, one group with high blood pressure ("hypertensive") and one with normal blood pressure ("normal").... All animals were then given antibiotics for 10 days to reduce their natural microbiota. After the course of antibiotics, the researchers transplanted hypertensive microbiota to normal blood pressure rats mice and normal microbiota to the hypertensive group.
The researchers found that the group treated with hypertensive microbiota developed elevated blood pressure. A more surprising result is that the rats mice treated with normal microbiota did not have a significant drop in blood pressure, although readings did decrease slightly. This finding is "further evidence for the continued study of the microbiota in the development of hypertension in humans and supports a potential role for probiotics as treatment for hypertension," wrote the researchers. "Studies showing that supplementing the diet with probiotics (beneficial microorganisms found in the gut) can have modest effects on blood pressure, especially in hypertensive models."
NOTE that the actual study said in its CONCLUSIONS: "Taken together, we have described clearly the disordered profiles of gut microbiota and microbial products in human patients with pre-hypertension and hypertension, established the relationship between gut dysbiosis and hypertension, and provided important evidence for the novel role of gut microbiota dysbiosis as a key factor for blood pressure changes. Our findings point towards a new strategy aimed at preventing the development of hypertension and reducing cardiovascular risks through restoring the homeostasis of gut microbiota, by improving diet and lifestyle or early intervening with drugs or probiotics."

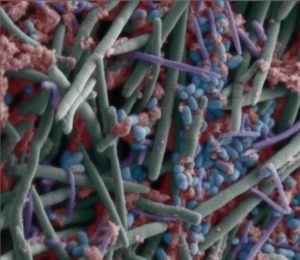 Gut bacteria in children varies among different Asian countries. A
Gut bacteria in children varies among different Asian countries. A  Human lungs. Credit: Wikipedia
Human lungs. Credit: Wikipedia