 A recent study has examined the issue of whether the 10 to 1 ratio of bacteria to human cells, which is widely quoted, is actually correct. Weizmann Institute of Science researchers currently feel that based on scientific evidence (which of course will change over time) and making "educated estimates", the actual ratio is closer to 1:1 (but overall there still are more bacterial than human cells). They point out that the 10:1 ratio was originally a "back of the envelope" estimate dating back to 1972.
A recent study has examined the issue of whether the 10 to 1 ratio of bacteria to human cells, which is widely quoted, is actually correct. Weizmann Institute of Science researchers currently feel that based on scientific evidence (which of course will change over time) and making "educated estimates", the actual ratio is closer to 1:1 (but overall there still are more bacterial than human cells). They point out that the 10:1 ratio was originally a "back of the envelope" estimate dating back to 1972.
The researchers also point out that the ratio may vary over the course of each day - as a person defecates out huge amounts of bacteria with each bowel movement. However, this study - which is not the final word - is an educated guess about bacteria only. What about the viruses, the fungi, etc that also reside on and within us? We know much less about all the other microbes. I am disturbed that article after article, and headline after headline, equates microbes and bacteria. Microbes does not mean only bacteria. From Science Daily:
Germs, humans and numbers: New estimate revises our microbiome numbers downwards
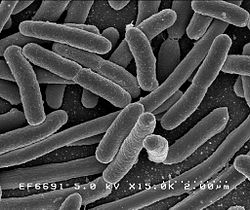
How many microbes inhabit our body on a regular basis? For the last few decades, the most commonly accepted estimate in the scientific world puts that number at around ten times as many bacterial as human cells. In research published in the journal Cell, a recalculation of that number by Weizmann Institute of Science researchers reveals that the average adult has just under 40 trillion bacterial cells and about 30 trillion human ones, making the ratio much closer to 1:1.
The rising importance of the microbiome in current scientific research led the Weizmann Institute's Prof. Ron Milo, Dr. Shai Fuchs and research student Ron Sender to revisit the common wisdom concerning the ratio of "personal" bacteria to human cells.
The original estimate that bacterial cells outnumber human cells in the body by ten to one was based on, among other things, the assumption that the average bacterium is about 1,000 times smaller than the average human cell. The problem with this estimate is that human cells vary widely in size, as do bacteria. For example, red blood cells are at least 100 times smaller than fat or muscle cells, and the microbes in the large intestine are about four times the size of the often-used "standard" bacterial cell volume. The Weizmann Institute scientists weighted their computations by the numbers of the different-sized human cells, as well as those of the various microbiome cells.
Some excerpts from the original journal article from Cell: Are We Really Vastly Outnumbered? Revisiting the Ratio of Bacterial to Host Cells in Humans
The human microbiome has emerged as an area of utmost interest....One of the most fundamental and commonly cited figures in this growing field is the estimate that bacteria residing in the human body outnumber human cells by a factor of 10 or more (Figure 1A). This striking statement often serves as an entry point to the field. After all, if a human being is a cell population composed of at least 90% bacteria, it is only natural to expect a major role for them in human physiology.
Both the numerator (number of microbial cells) and the denominator (human cells) of this 10:1 ratio are based on crude assessments. Most sources cite the number of human cells as 1013 or 1014.....We performed a thorough review of the literature and found a long chain of citations originating from one “back of the envelope” estimate (Figure 1). This estimate, though illuminating, was never meant as the final word on the question.
Recently, the estimate of a 10:1 bacterial to human cell ratio (B/H) ratio has received criticism (Rosner, 2014). Therefore, an alternative value and an estimate of the uncertainty range are needed. Bacteria are found in many parts of the human body primarily on the external and internal surfaces, including the gastrointestinal tracts, skin, saliva, oral mucosa, and conjunctiva. The vast majority of commensal bacteria reside in the colon, with previous estimates of about 1014 bacteria (Savage, 1977), followed by the skin, which is estimated to harbor ∼1012 bacteriaBerg, 1996). Less than 1012 bacteria populate the rest of the body.....Almost all recent papers in the field of gut microbiota directly or indirectly rely on a single paper (Savage, 1977) discussing the overall number of bacteria in the gut. Interestingly, review of the original Savage 1977 paper demonstrates that it actually cites another paper for the estimate (Luckey, 1972)....The estimate, performed by Luckey in 1972, is an illuminating example of a back-of-the-envelope estimate, which was elegantly performed, yet was probably never meant to serve as the cornerstone reference number to be cited decades later.
Updating the ratio of bacteria to human cells from 10:1 or 100:1 to closer to 1:1 does not take away from the biological importance of the microbiota. ...Although we still appear to be outnumbered, we now know more reliably to what degree and can quantify our uncertainty about the ratios and absolute numbers. The B/H ratio is actually close enough to one, so that each defecation event, which excretes about 1/3 of the colonic bacterial content, may flip the ratio to favor human cells over bacteria. This anecdote serves to highlight that some variation in the ratio of bacterial to human cells occurs not only across individual humans but also over the course of the day.

 Now and then I hear people wondering whether the many hours we spend staring at computer, cell phone, and tablet screens is damaging our eyes. And what about fluorescent lighting (which seems to bother many people) and LED lights? After all, the blue light of all our device screens seems intense, and researchers have long known that blue light is toxic to the retina.
Now and then I hear people wondering whether the many hours we spend staring at computer, cell phone, and tablet screens is damaging our eyes. And what about fluorescent lighting (which seems to bother many people) and LED lights? After all, the blue light of all our device screens seems intense, and researchers have long known that blue light is toxic to the retina. This study is noteworthy and relevant to humans (it was done on mice) because it may explain why so many people taking antibiotics get frequent viruses or seem more susceptible to infections. Once bacteria (both good and bad) are killed by antibiotics, then the community becomes unbalanced (dysbiosis), so that viruses may gain a foothold and a viral infection develops. In a healthy microbial community all sorts of microbes can be found, even ones we typically consider pathogenic, but the whole community keeps them in balance. One can say that "depletion of commensal microbiota also affects antiviral immunity".
This study is noteworthy and relevant to humans (it was done on mice) because it may explain why so many people taking antibiotics get frequent viruses or seem more susceptible to infections. Once bacteria (both good and bad) are killed by antibiotics, then the community becomes unbalanced (dysbiosis), so that viruses may gain a foothold and a viral infection develops. In a healthy microbial community all sorts of microbes can be found, even ones we typically consider pathogenic, but the whole community keeps them in balance. One can say that "depletion of commensal microbiota also affects antiviral immunity". Once again, research shows that "BPA-free" plastic does not mean it is safer than BPA plastic. Both BPA and BPS (the usual replacement for BPA) leach estrogenic chemicals into the foods and beverages, which means negative health effects when ingested. Both BPA and BPS mimic the effects of estrogen, as well as the actions of thyroid hormone. Yes, this study was done on zebrafish, but think of them as "the canaries in the mine" - if it affects them, it could affect humans also, especially developing fetuses and young children.
Once again, research shows that "BPA-free" plastic does not mean it is safer than BPA plastic. Both BPA and BPS (the usual replacement for BPA) leach estrogenic chemicals into the foods and beverages, which means negative health effects when ingested. Both BPA and BPS mimic the effects of estrogen, as well as the actions of thyroid hormone. Yes, this study was done on zebrafish, but think of them as "the canaries in the mine" - if it affects them, it could affect humans also, especially developing fetuses and young children. I posted about this amazing research while it was still ongoing (
I posted about this amazing research while it was still ongoing ( It's now 3 years being free of chronic sinusitis and off all antibiotics! Three amazing years since I started using easy do-it-yourself sinusitis treatments containing the probiotic (beneficial bacteria) Lactobacillus sakei. My sinuses feel great! And yes, it still feels miraculous.
It's now 3 years being free of chronic sinusitis and off all antibiotics! Three amazing years since I started using easy do-it-yourself sinusitis treatments containing the probiotic (beneficial bacteria) Lactobacillus sakei. My sinuses feel great! And yes, it still feels miraculous. Why exercise alone won't get those pounds off - it's because the body adapts to higher exercise levels. We all suspected that, but it is depressing... From Medical Xpress:
Why exercise alone won't get those pounds off - it's because the body adapts to higher exercise levels. We all suspected that, but it is depressing... From Medical Xpress:
 This confirms what researchers such as
This confirms what researchers such as  Once again, two opposing views about beards have been in the news - that they harbor all sorts of nasty disease-causing bacteria vs they are hygienic. An earlier
Once again, two opposing views about beards have been in the news - that they harbor all sorts of nasty disease-causing bacteria vs they are hygienic. An earlier