An argument for the need for human exposure to the microbes in rural environments. However, the role of diesel exhaust and other urban air pollutants is not discussed here (for example, diesel exhaust is linked to asthma). From Science Daily:
Rural microbes could boost city dwellers' health, study finds
The greater prevalence of asthma, allergies and other chronic inflammatory disorders among people of lower socioeconomic status might be due in part to their reduced exposure to the microbes that thrive in rural environments, according to a new scientific paper co-authored by a University of Colorado Boulder researcher.
The article, published in the journal Clinical & Experimental Immunology, argues that people living in urban centers who have less access to green spaces may be more apt to have chronic inflammation, a condition caused by immune system dysfunction.
When our immune systems are working properly, they trigger inflammation to fight off dangerous infections, but the inflammation disappears when the infection is gone. However, a breakdown in immune system function can cause a low level of inflammation to persist indefinitely. Such chronic inflammation can cause a host of health disorders.
Some scientists have hypothesized that the increase of chronic inflammation in wealthier Western countries is connected to lifestyles that have essentially become too clean. The so-called "hygiene hypothesis" is based on the notion that some microbes and infections interact with the immune system to suppress inflammation and that eliminating exposure to those things could compromise your health.
The authors agree that microbes and some types of infections are important because they can keep the immune system from triggering inflammation when it's not necessary, as happens with asthma attacks and allergic reactions.
But they say the infections that were historically important to immune system development have largely been eliminated in developed countries. The modern diseases we pick up from school, work and other crowded areas today do not actually lead to lower instances of inflammatory disorders.
During our evolutionary history, the human immune system was exposed to microbes and infections in three important ways: commensal microbes were passed to infants from their mothers and other family members; people came into contact with nonpathogenic microbes in the environment; and people lived with chronic infections, such as helminths, which are parasitic worms found in the gut and blood.
In order for those "old infections" to be tolerated in the body for long periods of time, they evolved a mechanism to keep the human immune system from triggering inflammation. Similarly, environmental bacteria, which were abundant and harmless, were tolerated by the immune system. According to Rook, a professor at UCL, "Helminthic parasites need to be tolerated by the immune system because, although not always harmless, once they are established in the host efforts by the immune system to eliminate them are futile, and merely cause tissue damage."
In contrast, relatively modern "crowd infections," such as measles or chicken pox, cause an inflammatory response. The result is that either the sick person dies or the infection is wiped out by the inflammation and the person becomes immune from having the same infection again in the future.
Collectively, the authors refer to the microbes and old infections that had a beneficial impact on the function of our immune systems as "old friends." Exposure to old friends plays an important role in guarding against inflammatory disorders, the authors said. Because the "old infections" are largely absent from the developed world, exposure to environmental microbes -- such as those found in rural environments, like farms and green spaces -- has likely become even more important.
The authors say this would explain why low-income urban residents -- who cannot easily afford to leave the city for rural vacations -- are more likely to suffer from inflammatory disorders. The problem is made worse because people who live in densely populated areas also are more likely to contract crowd infections, which cause more inflammation.
 It has been known for a while that getting a good night's sleep after getting vaccinated results in a stronger immune response. Twice as strong response! A recent study suggests that this could be due to beneficial T-cells (which are part of immune system) migrating toward the lymph nodes during sleep.
It has been known for a while that getting a good night's sleep after getting vaccinated results in a stronger immune response. Twice as strong response! A recent study suggests that this could be due to beneficial T-cells (which are part of immune system) migrating toward the lymph nodes during sleep.

 We've known for a while that exposure to microbes during the baby's first year is important (and good) for the developing immune system. In addition, recent research suggests that during the second trimester of pregnancy the developing fetus already has microbes in its body which help "educate" the developing immune system.
We've known for a while that exposure to microbes during the baby's first year is important (and good) for the developing immune system. In addition, recent research suggests that during the second trimester of pregnancy the developing fetus already has microbes in its body which help "educate" the developing immune system.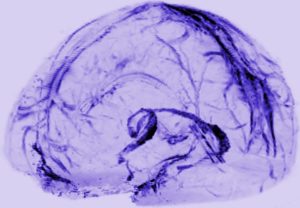 I can't resist posting excerpts from a recent article announcing that researchers just found an entirely new lymph system ("lymphatic vessels") in the brain that transports fluid in the brain, and is probably "crucial to metabolic and inflammatory processes". The image in this post shows the system in the brain. Amazing that it is only now "discovered" - apparently it was noticed by an anatomist 2 centuries ago, but this was pooh-poohed by modern day physicians. Until now. Excerpts from the Atlantic:
I can't resist posting excerpts from a recent article announcing that researchers just found an entirely new lymph system ("lymphatic vessels") in the brain that transports fluid in the brain, and is probably "crucial to metabolic and inflammatory processes". The image in this post shows the system in the brain. Amazing that it is only now "discovered" - apparently it was noticed by an anatomist 2 centuries ago, but this was pooh-poohed by modern day physicians. Until now. Excerpts from the Atlantic: Some studies with humans suggest that cancer growth is slowed with exercise, better cancer prognosis with regular exercise, and lowered cancer recurrence (e.g., exercise after prostate cancer diagnosis), but a recent study looked at the issue more in depth.
Some studies with humans suggest that cancer growth is slowed with exercise, better cancer prognosis with regular exercise, and lowered cancer recurrence (e.g., exercise after prostate cancer diagnosis), but a recent study looked at the issue more in depth.