 Nowadays there is tremendous concern about the spread of antibiotic resistant bacteria or "superbugs" throughout the world. Articles frequently mention India being at the epicenter of this crisis - that is, the source of many antibiotic resistant strains (both in and out of hospitals), which then travel throughout the world due to global travel. The massive overuse and misuse of antibiotics (whether in humans, animals, and even crops) is usually given as the major reason for the development of antibiotic resistant strains of bacteria (here, here, and here).
Nowadays there is tremendous concern about the spread of antibiotic resistant bacteria or "superbugs" throughout the world. Articles frequently mention India being at the epicenter of this crisis - that is, the source of many antibiotic resistant strains (both in and out of hospitals), which then travel throughout the world due to global travel. The massive overuse and misuse of antibiotics (whether in humans, animals, and even crops) is usually given as the major reason for the development of antibiotic resistant strains of bacteria (here, here, and here).
Thus the following article about unchecked pollution from pharmaceutical companies in India fueling the creation of deadly superbugs was shocking to read - and it may explain why the problem is so severe there. Note that the Indian companies supply just about all the world's major drug companies with antibiotics and anti-fungals. It appears that the companies are ignoring local laws (which have been called "toothless") which would cut down on the pollution. What is stressed in the article is that one of the world’s biggest drug production hubs (the Indian city of Hyderabad) is producing dangerous levels of pharmaceutical pollution, and the international agencies that ensure drug safety are basically ignoring this problem (and doing little to address it).
Thousands of tons of pharmaceutical waste is produced each day by the many pharmaceutical companies in Hyderabad, India, which is then contaminating the water sources in the area. With the result that water samples (from rivers, lakes, groundwater, drinking water, surface water, treated sewage water) in that area contain bacteria and fungi resistant to multiple drugs (superbugs), and these superbugs then get spread to humans throughout India and eventually globally. This article is definitely worth reading in its entirety. Excerpts from The Bureau of Investigative Journalism:
Big Pharma's Pollution Is Creating Deadly Superbugs While The World Looks The Other Way
Industrial pollution from Indian pharmaceutical companies making medicines for nearly all the world’s major drug companies is fueling the creation of deadly superbugs, suggests new research. Global health authorities have no regulations in place to stop this happening. A major study published today in the prestigious scientific journal Infection found “excessively high” levels of antibiotic and antifungal drug residue in water sources in and around a major drug production hub in the Indian city of Hyderabad, as well as high levels of bacteria and fungi resistant to those drugs. Scientists told the Bureau the quantities found meant they believe the drug residues must have originated from pharmaceutical factories.
The presence of drug residues in the natural environment allows the microbes living there to build up resistance to the ingredients in the medicines that are supposed to kill them, turning them into what we call superbugs. The resistant microbes travel easily and have multiplied in huge numbers all over the world, creating a grave public health emergency that is already thought to kill hundreds of thousands of people a year.
When antimicrobial drugs stop working common infections can become fatal, and scientists and public health leaders say the worsening problem of antibiotic resistance (also known as AMR) could reverse half a century of medical progress if the world does not act fast. Yet while policies are being put into place to counter the overuse and misuse of drugs which has propelled the crisis, international regulators are allowing dirty drug production methods to continue unchecked. Global authorities like the Food and Drug Administration and the European Medicines Agency strictly regulate drug supply chains in terms of drug safety - but environmental standards do not feature in their rulebook. Drug producers must adhere to Good Manufacturing Practices (GMP) guidelines - but those guidelines do not cover pollution.
The international bodies say the governments of the countries where the drugs are made are the ones responsible for stopping pollution - but domestic legislation is having little impact on the ground, say the study's authors. The lack of international regulation must be addressed, they argue, highlighting the grave public health threat faced by antibiotic resistance as well as the rampant global spread of superbugs from India, which has become an epicentre of the crisis.
A group of scientists based at the University of Leipzig worked with German journalists to take an in-depth look at pharmaceutical pollution in Hyderabad, where 50% of India’s drug exports are produced. A fifth of the world’s generic drugs are produced in India, with factories based in Hyderabad supplying Big Pharma and public health authorities like World Health Organisation with millions of tons of antibiotics and antifungals each year.
The researchers tested 28 water samples in and around the Patancheru-Bollaram Industrial zone on the outskirts of the city, where more than than 30 drug manufacturing companies supplying nearly all the world’s major drug companies are based. Thousands of tons of pharmaceutical waste are produced by the factories each day, the paper says. Almost all the samples contained bacteria and fungi resistant to multiple drugs (known as MDR pathogens, the technical name for superbugs). Researchers then tested 16 of the samples for drug residues and found 13 of them were contaminated with antibiotics and antifungals. Previous studies have shown how exposure to antibiotics and antifungals in the environment causes bacteria and fungi to develop immunity to those drugs.
Environmental pollution and poor management of wastewater in Hyderabad is causing “unprecedented antimicrobial drug contamination” of surrounding water sources, conclude the researchers - contamination which appears to be driving the creation and spread of dangerous superbugs which have spread across the world. Combined with the mass misuse of antibiotics and poor sanitation, superbugs are already having severe consequences in India - an estimated 56,000 newborn babies die from resistant infections there each year.
The companies in question strongly deny that their factories pollute the environment, and the sheer number of factories operating in Hyderabad means it is impossible to identify exactly which companies are responsible for the contamination found in the samples tested. What is clear is one of the world’s biggest drug production hubs is producing dangerous levels of pharmaceutical pollution, and the international bodies tasked with ensuring drug safety are doing little to address it.
Around 170 companies making bulk drugs like antibiotics operate in and around Hyderabad, the majority clustered in sprawling industrial estates along the banks of the Musi river. Companies in Europe and the US, as well as health authorities like WHO and the UK’s NHS are reliant on drugs being produced in these factories.
The area has long been criticised for its pollution, which has continued unabated despite decades of campaigning by Indian NGOs, say the report authors. In 2009 the Patancheru-Bollaram zone was classified as “critically polluted” in India’s national pollution index and construction in the area was banned. But the government relaxed the rules in 2014 and building was allowed to begin again. Last year India’s Supreme Court ordered the country’s pharmaceutical companies to operate a zero liquid waste policy, but “massive violations” have reportedly occurred, says the Infection report....India has become the epicentre of the global drug resistance crisis, with 56,000 newborn Indian babies estimated to die each year from drug-resistant blood infections, and 70 to 90% of people who travel to India returning home with multi-drug-resistant bacteria in their gut, according to the study.
Researchers took water samples from rivers, lakes, groundwater, drinking water and surface water from rural and urban areas in and around the industrial estate, as well as pools near factories and water sources contaminated by sewage treatment plants. Four were taken from taps, one from a borehole, and the remaining 23 were classed as environmental samples. The samples were tested for bacteria resistant to multiple drugs (known as MDR pathogens, the technical name for superbugs). The researchers then tested 16 of the samples for the antibiotics and antifungals used to treat infections. All samples apart from one taken from tap water at a four star hotel were found to contain drug-resistant bacteria. All 23 environmental samples contained carbapenemase-producing bacteria - a group of bugs dubbed the “nightmare bacteria” because they are virtually untreatable and kill 40-50% of people whose blood gets infected with them.
Of the 16 samples then tested for drug residue, 13 were found to be contaminated with antibiotics and antifungals, some in disturbingly high levels. The researchers compared the levels of residue to limits recommended by leading microbiologists; once levels exceed those limits it is likely that superbugs will develop. The amounts of antimicrobials found in the new tests were “eye-wateringly high”, said Dr Mark Holmes, a microbiologist at the University of Cambridge. “The quantities involved mean the amount in the water is almost the same as a therapeutic dose,” he said, calling on the Indian authorities to investigate immediately by testing each factory’s effluent.
There are reams of regulations and stipulations that manufacturers have to adhere to in order to export their products to the US and Europe – known as the Good Manufacturing Practices (GMP) framework. These focus on making sure drugs are safe, pure, and effective. Stringent inspections by the FDA, WHO and European authorities check that these rules are being followed. However these regulations do not address environmental concerns. Inspectors have no mandate to sanction a factory for polluting, failing to treat its waste or other environmental problems – this falls within the remit of local governments.
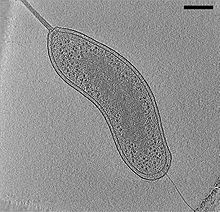
 The following article is about Dr. Janelle Ayres, a researcher in California, working on "beneficial bacteria" to help the body tolerate infections. This is different than the usual medical approach of fighting infections - where antibiotics are used to kill microbes. Reading the article, my first thought was "Well, duh....of course this approach works." This is what we've been doing in using Lactobacillus sakei, a beneficial bacteria, in successfully treating sinusitis since early 2013! ..... The good news in reading this article is that using bacteria to treat infections or diseases seems to finally be going mainstream.
The following article is about Dr. Janelle Ayres, a researcher in California, working on "beneficial bacteria" to help the body tolerate infections. This is different than the usual medical approach of fighting infections - where antibiotics are used to kill microbes. Reading the article, my first thought was "Well, duh....of course this approach works." This is what we've been doing in using Lactobacillus sakei, a beneficial bacteria, in successfully treating sinusitis since early 2013! ..... The good news in reading this article is that using bacteria to treat infections or diseases seems to finally be going mainstream.
 Great idea and one that this blog has been pushing for a long time - the use of
Great idea and one that this blog has been pushing for a long time - the use of  Nowadays there is tremendous concern about the spread of antibiotic resistant bacteria or "superbugs" throughout the world. Articles frequently mention India being at the epicenter of this crisis - that is, the source of many antibiotic resistant strains (both in and out of hospitals), which then travel throughout the world due to global travel. The massive overuse and misuse of antibiotics (whether in humans, animals, and even crops) is usually given as the major reason for the development of antibiotic resistant strains of bacteria (
Nowadays there is tremendous concern about the spread of antibiotic resistant bacteria or "superbugs" throughout the world. Articles frequently mention India being at the epicenter of this crisis - that is, the source of many antibiotic resistant strains (both in and out of hospitals), which then travel throughout the world due to global travel. The massive overuse and misuse of antibiotics (whether in humans, animals, and even crops) is usually given as the major reason for the development of antibiotic resistant strains of bacteria (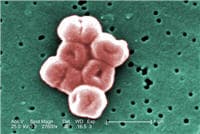 Many posts on this blog are about beneficial microbes, and the many species of microbes (bacteria, fungi, viruses) living within and on us. But there are also bacteria in the world that pose a serious threat to human health, and the list of these are growing due to antibiotic resistance. This week the World Health Organization (WHO) officials came out with a list of a dozen antibiotic-resistant "priority pathogens" that pose the greatest threats to human health. These are bacteria resistant to multiple antibiotics - thus superbugs.
Many posts on this blog are about beneficial microbes, and the many species of microbes (bacteria, fungi, viruses) living within and on us. But there are also bacteria in the world that pose a serious threat to human health, and the list of these are growing due to antibiotic resistance. This week the World Health Organization (WHO) officials came out with a list of a dozen antibiotic-resistant "priority pathogens" that pose the greatest threats to human health. These are bacteria resistant to multiple antibiotics - thus superbugs.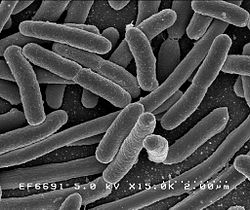 A few days ago the CDC (Centers for Disease Control and Prevention) released
A few days ago the CDC (Centers for Disease Control and Prevention) released  The big scary question: What will happen after antibiotics cease to work? And people start dying by the millions from infections that used to be easily treated? We are fast approaching that point of total antibiotic resistance, with superbugs that resist all antibiotics. More and more disease-causing bacteria are rapidly evolving immunity to every existing antibiotic (see
The big scary question: What will happen after antibiotics cease to work? And people start dying by the millions from infections that used to be easily treated? We are fast approaching that point of total antibiotic resistance, with superbugs that resist all antibiotics. More and more disease-causing bacteria are rapidly evolving immunity to every existing antibiotic (see