.jpg) There are some things we can do that are linked to living longer, such as not smoking and exercising regularly, but could reading books also have such an effect? A study published in the journal Social Science and Medicine concludes that those who regularly read books add several years to their lives. They found this effect in both men and women, found that reading books are "protective regardless of gender, wealth, education", but the effect holds only for books and not magazines and newspapers. Since surveys show that 87% of book readers read fiction, then it is likely that most of the book readers were reading fiction.
There are some things we can do that are linked to living longer, such as not smoking and exercising regularly, but could reading books also have such an effect? A study published in the journal Social Science and Medicine concludes that those who regularly read books add several years to their lives. They found this effect in both men and women, found that reading books are "protective regardless of gender, wealth, education", but the effect holds only for books and not magazines and newspapers. Since surveys show that 87% of book readers read fiction, then it is likely that most of the book readers were reading fiction.
In the long-term (12 years) study of 3,635 people, the researchers found that those that read books for more than 3.5 hours per week lived on average two years longer than non-readers, and that there was a dose-response effect (the more one reads, the better). This appeared to be linked to cognitive enhancement rather than any other associated factor, such as age, sex, education, race, health, wealth, etc. The research team from the Yale University School of Public Health divided their subjects into three groups: those who didn’t read at all, those who read for 3.5 hours per week or less, and those who read for more than 3.5 hours per week. They found that the occasional readers were 17 percent less likely to die during the follow-up period than those who did not. This beneficial effect of reading was only linked to books, and not other forms of reading material such as magazines or newspapers. From the journal Social Science and Medicine:
A chapter a day: Association of book reading with longevity
This study examined whether those who read books have a survival advantage over those who do not read books and over those who read other types of materials, and if so, whether cognition mediates this book reading effect. The cohort consisted of 3635 participants in the nationally representative Health and Retirement Study who provided information about their reading patterns at baseline.....based on survival information up to 12 years after baseline. A dose-response survival advantage was found for book reading by tertile.....Book reading contributed to a survival advantage that was significantly greater than that observed for reading newspapers or magazines. Compared to non-book readers, book readers had a 23-month survival advantage at the point of 80% survival in the unadjusted model. A survival advantage persisted after adjustment for all covariates (HR = .80, p < .01), indicating book readers experienced a 20% reduction in risk of mortality over the 12 years of follow up compared to non-book readers. Cognition mediated the book reading-survival advantage. These findings suggest that the benefits of reading books include a longer life in which to read them.
While most sedentary behaviors are well-established risk factors for mortality in older individuals (Wullems et al., 2016; de Rezenade et al., 2014, Katzmaryk & Lee, 2012; Muennig, Rosen, & Johnson, 2013), previous studies of a behavior which is often sedentary, reading, have had mixed outcomes....We speculated that books engage readers’ minds more than newspapers and magazines, leading to cognitive benefits that drive the effect of reading on longevity.
Reading books tends to involve two cognitive processes that could create a survival advantage. First, it promotes "deep reading,” which is a slow, immersive process; this cognitive engagement occurs as the reader draws connections to other parts of the material, finds applications to the outside world, and asks questions about the content presented (Wolf, Barzillai, & Dunne, 2009). Cognitive engagement may explain why vocabulary, reasoning, concentration, and critical thinking skills are improved by exposure to books (Stanovich, West, & Harrison, 1995; Stanovich & Cunningham, 1998; Wolf, Barzillai, & Dunne, 2009). Second, books can promote empathy, social perception, and emotional intelligence, which are cognitive processes that can lead to greater survival (Bassuk, Wypij, & Berkmann, 2000; Djikic, Oatley, & Moldoveanu 2013; Kidd & Castano 2013; Shipley, Der, Taylor, & Deary 2008; Olsen, Olsen, Gunner-Svensson, & Waldstrom, 1991).
The final sample consisted of 3635 individuals that were followed over 34,496 person years, with 27.4% of the sample dying during an average 9.49 years of follow-up. Consistent with the older population, the sample was predominantly (62%) female.....The average time spent reading per week was 3.92 hours for books and 6.10 hours for periodicals. The two types of reading were not strongly correlated, and 38% of the sample (n=1390) read only books or only periodicals; this allowed them to be treated as separate constructs.....Cognitive engagement was assessed with total cognitive score (available in the supplemental Imputation of Cognitive Function Measures) which is a summary variable based on 8 items, including immediate recall, delayed recall, serial 7s, backwards count from 20, object naming, President naming, Vice President naming, and date naming.
A 20% reduction in mortality was observed for those who read books, compared to those who did not read books. Further, our analyses demonstrated that any level of book reading gave a significantly stronger survival advantage than reading periodicals.....The mediation analyses showed for the first time that the survival advantage was due to the effect that book reading had on cognition....This finding suggests that reading books provide a survival advantage due to the immersive nature that helps maintain cognitive status.

 It has long been known that laser pointers can be damaging to the eyes, but apparently this is not widely known. Injuries to the eyes (retinal injuries) causing irreversible vision loss are rapidly increasing from them, especially among children. Injuries to the eye happen when a person stares directly into the laser pointer, or even into the reflection in a mirror. This can inadvertently happen among children, for example when playing games such as laser tag.
It has long been known that laser pointers can be damaging to the eyes, but apparently this is not widely known. Injuries to the eyes (retinal injuries) causing irreversible vision loss are rapidly increasing from them, especially among children. Injuries to the eye happen when a person stares directly into the laser pointer, or even into the reflection in a mirror. This can inadvertently happen among children, for example when playing games such as laser tag. The latest development in treating stubborn cases of Clostridium difficile infections (CDI) are "poop pills" - pills that patients can easily swallow rather than having to go through a fecal microbiota transplant (FMT). The "poop pills" are filled with blenderized fecal matter from healthy donors, are much easier for patients to swallow, and they successfully treat C. difficile at almost the same rate as fecal microbiota transplants - about 91% after 1 or 2 treatments for the pills, and 93 to 96% for FMT. This is an amazing success rate for an infection that debilitates people, is resistant to antibiotics in many cases, and even kills people.
The latest development in treating stubborn cases of Clostridium difficile infections (CDI) are "poop pills" - pills that patients can easily swallow rather than having to go through a fecal microbiota transplant (FMT). The "poop pills" are filled with blenderized fecal matter from healthy donors, are much easier for patients to swallow, and they successfully treat C. difficile at almost the same rate as fecal microbiota transplants - about 91% after 1 or 2 treatments for the pills, and 93 to 96% for FMT. This is an amazing success rate for an infection that debilitates people, is resistant to antibiotics in many cases, and even kills people.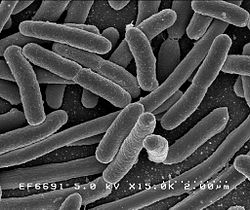 Here is an amazing short video for those interested in seeing how bacteria mutate and grow when exposed to antibiotics - and evolving to become superbugs. Researchers filmed an experiment that created bacteria a thousand times more drug-resistant than their ancestors. In the time-lapse video, a white bacterial colony (E.coli bacteria) creeps across an enormous black petri dish plated with vertical bands of successively higher doses of antibacterial drugs (antibiotics).
Here is an amazing short video for those interested in seeing how bacteria mutate and grow when exposed to antibiotics - and evolving to become superbugs. Researchers filmed an experiment that created bacteria a thousand times more drug-resistant than their ancestors. In the time-lapse video, a white bacterial colony (E.coli bacteria) creeps across an enormous black petri dish plated with vertical bands of successively higher doses of antibacterial drugs (antibiotics). Over the years I have read about some oils, especially lavender and tea tree oils, as having hormone altering (endocrine disrupting) effects when used over prolonged periods of time or when someone is "chronically exposed". Especially worrisome was the possible estrogenic effects of lavender oils in shampoos, lotions, and soaps on developing children - especially boys (prolonged use leading to the development of breasts in some boys!). I just read a recently published journal study (with very interesting comments at the end), and an article in WebMD about this same topic. The condition of early breast development is called prepubertal gynecomastia in boys and thelarche in girls.
Over the years I have read about some oils, especially lavender and tea tree oils, as having hormone altering (endocrine disrupting) effects when used over prolonged periods of time or when someone is "chronically exposed". Especially worrisome was the possible estrogenic effects of lavender oils in shampoos, lotions, and soaps on developing children - especially boys (prolonged use leading to the development of breasts in some boys!). I just read a recently published journal study (with very interesting comments at the end), and an article in WebMD about this same topic. The condition of early breast development is called prepubertal gynecomastia in boys and thelarche in girls. This article by Dr. Thomas E. Finucane lays out nicely a paradigm shift in how to view uncomplicated urinary tract infections (UTIs) - as a case of dysbiosis (microbial community out of whack), and that antibiotics to kill bacteria are generally not needed or helpful. (He doesn't mention it, but the next step in his argument should be that probiotic or beneficial bacteria or other microbes may improve the microbial community and symptoms.) A main point of the article is that we now know the urinary tract is not sterile - instead diverse microbiota live there (the microbial community is the
This article by Dr. Thomas E. Finucane lays out nicely a paradigm shift in how to view uncomplicated urinary tract infections (UTIs) - as a case of dysbiosis (microbial community out of whack), and that antibiotics to kill bacteria are generally not needed or helpful. (He doesn't mention it, but the next step in his argument should be that probiotic or beneficial bacteria or other microbes may improve the microbial community and symptoms.) A main point of the article is that we now know the urinary tract is not sterile - instead diverse microbiota live there (the microbial community is the  A new study conducted in China found an association between low vitamin D levels and future cognitive decline in older adults. The lower the vitamin D levels at the initial screening (the baseline), the more people with cognitive decline at a 2 year follow-up. There were were no gender differences. (
A new study conducted in China found an association between low vitamin D levels and future cognitive decline in older adults. The lower the vitamin D levels at the initial screening (the baseline), the more people with cognitive decline at a 2 year follow-up. There were were no gender differences. ( A lot of research has shown benefits to being bilingual (
A lot of research has shown benefits to being bilingual ( Yikes! Another study showing effects from antibiotic use - this time a higher incidence of food allergies in children who took antibiotics in the first year of life. Especially multiple courses of antibiotics, with the strongest association among children receiving cephalosporin and sulfonamide antibiotics. Antibiotics can be life-saving, but there can also be unintended consequences.
Yikes! Another study showing effects from antibiotic use - this time a higher incidence of food allergies in children who took antibiotics in the first year of life. Especially multiple courses of antibiotics, with the strongest association among children receiving cephalosporin and sulfonamide antibiotics. Antibiotics can be life-saving, but there can also be unintended consequences. A
A