 Just read a small study that compared the microbes in the sinus microbiome between 12 healthy people with no sinusitis (controls) and 14 with chronic sinusitis, their neurotransmitter levels (serotonin, dopamine, and GABA), and also looked at depression scores in the 2 groups. Well, of course they found some microbial differences between healthy people and those with chronic rhinosinusitis (CRS), but they also found that those with the most severe chronic sinusitis tended to have the most depressive symptoms, and lower amounts of the neurotransmitters studied, but they did not find significant differences overall.
Just read a small study that compared the microbes in the sinus microbiome between 12 healthy people with no sinusitis (controls) and 14 with chronic sinusitis, their neurotransmitter levels (serotonin, dopamine, and GABA), and also looked at depression scores in the 2 groups. Well, of course they found some microbial differences between healthy people and those with chronic rhinosinusitis (CRS), but they also found that those with the most severe chronic sinusitis tended to have the most depressive symptoms, and lower amounts of the neurotransmitters studied, but they did not find significant differences overall.
I found their summary and conclusions problematic, since they discussed that "possibly" the sinus microbes influence brain neurotransmitters. And they pointed out that as certain disease associated microbes increased (especially Moraxella), the neurotransmitter concentrations tended to decrease in those with sinusitis. But since there were no significant group differences, they did not prove their hypotheses, and conclusions can not be made. So saying there is "the potential for downstream effects of the sinonasal microbiota on neural signaling and, subsequently, brain function and behavior" is misleading and overreaching. The researchers also said it was "difficult to discern disease associations from natural variation." Hah!
It should be obvious that the worse the chronic sinusitis, the more depressive symptoms, because having chronic sinusitis is DEPRESSING. One suffers with it. Some people have told me how chronic sinusitis has destroyed their life - whether their health, financially, with relationships, etc. Of course they will have higher depressive scores! And when a Lactobacillus sakei product or other probiotic successfully treats sinusitis (usually very quickly), then the mood is one of elation as symptoms go away (finally health!).
All one can say (based on studies) is: the sinus microbiomes in healthy people (normal sinus microbial community) are somewhat different from those with chronic sinusitis (out-of-whack microbial community or dysbiosis). And one would expect that those with less severe/milder sinusitis have a "better" community of sinus microbes - that is, more microbes that are associated with health, and fewer of those associated with sickness, than sicker people. Which is what this study suggested. Excerpts from the International Forum of Allergy & Rhinology:
The sinonasal microbiota, neural signaling, and depression in chronic rhinosinusitis
The complex relationships between the human microbiota, the immune system, and the brain play important roles in both health and disease, and have been of increasing interest in the study of chronic inflammatory mucosal conditions. We hypothesized that the sinonasal microbiota may act as a modifier of interkingdom neural signaling and, subsequently, mental health, in the upper respiratory inflammatory condition chronic rhinosinusitis (CRS). In this study we investigated associations between the sinonasal microbiota; local concentrations of the neurotransmitters serotonin, dopamine, and γ-aminobutyric acid (GABA); and depression severity in a cohort of 14 CRS patients and 12 healthy controls.
Several commonly “health-associated” sinonasal bacterial taxa were positively associated with higher neurotransmitter concentrations and negatively associated with depression severity. In contrast, several taxa commonly associated with an imbalanced sinonasal microbiota negatively associated with neurotransmitters and positively with depression severity. Few significant differences were identified when comparing between control and CRS subject groups, including neurotransmitter concentrations, depression scores, or sinonasal microbiota composition or abundance. Conclusion: The findings obtained lend support to the potential for downstream effects of the sinonasal microbiota on neural signaling and, subsequently, brain function and behavior.
SOME OTHER EXCERPTS: Depression scores were also not significantly different between controls and CRS patients. .... The serotonin levels in CRS patients compared with control subjects tended to be lower, but not significantly so. Although median values for dopamine, GABA, and serotonin were generally lower in CRS patients than controls, all 3 neurotransmitters had a greater range among those with CRS, and no differences were significant. ... For both CRS and control individuals, bacterial communities were generally dominated by OTUs of the genera Corynebacterium and Staphylococcus.
Correlation analyses identified associations between members of the genera Staphylococcus, Finegoldia, Propionibacterium, Peptoniphilus, and Anaerococcus, as well as bacterial community diversity overall. Members of these genera have been previously identified as representative of more “health-associated” sinonasal bacterial community types, whereas their depletion has been associated with lower bacterial community diversity, increased bacterial load, increased rates of asthma, and elevated markers of inflammation. Similarly, members of the genera Burkholderia and Propionibacterium have been identified as 2 potential “gatekeepers” that help maintain bacterial community stability in the sinonasal tract. In the present study, several of these same bacterial taxa were significantly positively correlated with neurotransmitter levels and negatively with depression severity, whereas several other OTUs (including members of Streptococcus, Rothia, Enterobacteriaceae, Corynebacterium, and Moraxella) showed the opposite pattern (negatively associated with neurotransmitter levels and positively with depression severity).

 Last week a person told an
Last week a person told an  A new study has summarized what we know about fungi that live in and on babies - and yes, we all have fungi both on and within us. It's called the mycobiome. In healthy individuals all the microbes (bacteria, viruses, fungi, etc) live in balanced microbial communities, but the communities can become "out of whack" (dysbiosis) for various reasons, and microbes that formerly co-existed peacefully can multiply and become problematic. Or other pathogenic microbes can enter the community, and the person becomes ill.
A new study has summarized what we know about fungi that live in and on babies - and yes, we all have fungi both on and within us. It's called the mycobiome. In healthy individuals all the microbes (bacteria, viruses, fungi, etc) live in balanced microbial communities, but the communities can become "out of whack" (dysbiosis) for various reasons, and microbes that formerly co-existed peacefully can multiply and become problematic. Or other pathogenic microbes can enter the community, and the person becomes ill. What things in our environment have an effect on the microbes living within us? We now know that gut microbes are important for our health in many ways, and that
What things in our environment have an effect on the microbes living within us? We now know that gut microbes are important for our health in many ways, and that  A
A  This study is noteworthy and relevant to humans (it was done on mice) because it may explain why so many people taking antibiotics get frequent viruses or seem more susceptible to infections. Once bacteria (both good and bad) are killed by antibiotics, then the community becomes unbalanced (dysbiosis), so that viruses may gain a foothold and a viral infection develops. In a healthy microbial community all sorts of microbes can be found, even ones we typically consider pathogenic, but the whole community keeps them in balance. One can say that "depletion of commensal microbiota also affects antiviral immunity".
This study is noteworthy and relevant to humans (it was done on mice) because it may explain why so many people taking antibiotics get frequent viruses or seem more susceptible to infections. Once bacteria (both good and bad) are killed by antibiotics, then the community becomes unbalanced (dysbiosis), so that viruses may gain a foothold and a viral infection develops. In a healthy microbial community all sorts of microbes can be found, even ones we typically consider pathogenic, but the whole community keeps them in balance. One can say that "depletion of commensal microbiota also affects antiviral immunity". This article discusses the fungi living on our skin. Recent research (using state of the art genetic analysis) has found that healthy people have lots of diversity in fungi living on their skin. Certain areas seem to have the greatest populations of fungi:
This article discusses the fungi living on our skin. Recent research (using state of the art genetic analysis) has found that healthy people have lots of diversity in fungi living on their skin. Certain areas seem to have the greatest populations of fungi: 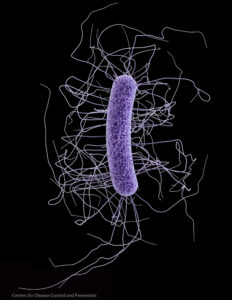 More research that supports that both more variety (diversity) of microbes and the actual mix of types of microbes are involved in a healthy
More research that supports that both more variety (diversity) of microbes and the actual mix of types of microbes are involved in a healthy