 Do you want to live longer and be healthy at the same time? Some possible ways may be to restrict the calories in the diet (every day) or to practice intermittent calorie restriction (a fasting mimicking diet a few days a month or even each week, such as the 5:2 diet). Previous studies in animals and humans have suggested that periodic fasting can reduce body fat, cut insulin levels, and provide other benefits. Studies in animals found that sharply restricting calories (calorie restriction or CR) daily resulted in longer, healthier lives, but it is unknown if the benefits of chronic calorie restriction also holds true for humans, and even if it might be dangerous. And really - how many people would actually want to reduce their calorie intake by 25% or more day in and day out for years? Intermittent calorie restriction seems much, much easier.
Do you want to live longer and be healthy at the same time? Some possible ways may be to restrict the calories in the diet (every day) or to practice intermittent calorie restriction (a fasting mimicking diet a few days a month or even each week, such as the 5:2 diet). Previous studies in animals and humans have suggested that periodic fasting can reduce body fat, cut insulin levels, and provide other benefits. Studies in animals found that sharply restricting calories (calorie restriction or CR) daily resulted in longer, healthier lives, but it is unknown if the benefits of chronic calorie restriction also holds true for humans, and even if it might be dangerous. And really - how many people would actually want to reduce their calorie intake by 25% or more day in and day out for years? Intermittent calorie restriction seems much, much easier.
Two recently published studies suggest health benefits of calorie restriction diets - chronic calorie restriction in adult rhesus monkeys, and intermittent calorie restriction (a fasting mimicking diet a few days a month) in humans.
Researchers at the Univ. of Wisconsin–Madison and National Institute of Aging reanalyzed two studies they had originally done with conflicting results, and now they reported in Nature Communications that chronic calorie restriction produced health benefits (such as lower incidence of cancer, cardiovascular problems) and longer life in rhesus monkeys. Since these primates have human-like aging patterns, they thought that CR would also have similar benefits in humans - a longer, healthier life. The researchers describe one monkey they started on a 30 percent calorie restriction diet when he was 16 years old (late middle age for rhesus monkeys), and that he is now 43 (a longevity record for the species). They found that in nonhuman primates calorie restriction is beneficial when started in adulthood (especially late middle age in males), but does not improve survival when started in juveniles (young animals) - and in fact they tended to die at an earlier age than the normal diet group of primates.
In the other study (in Science Translational Medicine), research suggests it is possible to gain anti-aging benefits with a “fasting-mimicking diet,” practiced just five days a month. 100 healthy adults (aged 20 to 70) were randomly assigned to either a group following a low-calorie "fasting-mimicking" diet (FMD) five days a month, for 3 months, or a normal diet control group. After 3 months, the control group also went on the fasting mimicking diet. Test subjects followed a 50 percent calorie restricted diet (totaling about 1,100 calories on the first day) and 70 percent diet (about 700 calories) on the next four days, then ate whatever they wanted for the rest of the month. The calorie-restricted diet was low in calories, sugars, and protein, was 100 percent plant-based, and featured vegetable soups, energy bars, energy drinks, and a chip snack, as well as mineral and vitamin supplements. (Note that Longo and Univ. of Southern California are both owners of L-Nutra, the company that manufactures the diet. But Longo says he takes no salary or consulting fees from the company.)
But it still wasn't easy for the test subjects to follow the 5 days of restricted calories per month because there was a 25% drop out rate. Health benefits (about a 6 pound weight loss, smaller waistlines, lower blood pressure, lower levels of inflammation, and better levels of glucose, triglycerides and cholesterol, etc.), showed up after the third month and persisted for at least three months—even after subjects had returned full-time to a normal diet. They lost body fat, but lean muscle mass remained unchanged. They found that the benefits were greater for people who were obese or otherwise unhealthy. In summary, the researchers said that 3 cycles of the 5 days per month of fasting-mimicking diet improved the levels of a variety of "markers/risk factors associated with poor health and aging and with multiple age-related diseases" (such as cancer, diabetes, heart disease, etc).
Other researchers say there is no need to suffer through such extreme diets, but to instead follow a healthy lifestyle, which includes a healthy diet (with lots of vegetables, fruits, legumes, seeds, whole grains, and nuts), and to exercise. And remember - nowhere does following restricted calorie diets mean you'll live longer - just that you should be healthier as you age (hopefully). There are no guarantees in life...
From Science Translational Medicine: Fasting-mimicking diet and markers/risk factors for aging, diabetes, cancer, and cardiovascular disease
Mice that fast periodically are healthier, metabolically speaking. To explore whether fasting can help people as well, Wei et al. studied 71 people who either consumed a fasting-mimicking diet for 5 days each month for 3 months or maintained their normal diet for 3 months and then switched to the fasting schedule. The fasting-like diet reduced body weight and body fat, lowered blood pressure, and decreased the hormone IGF-1, which has been implicated in aging and disease. A post hoc analysis replicated these results and also showed that fasting decreased BMI, glucose, triglycerides, cholesterol, and C-reactive protein (a marker for inflammation). These effects were generally larger in the subjects who were at greater risk of disease at the start of the study. A larger study is needed to replicate these results, but they raise the possibility that fasting may be a practical road to a healthy metabolic system.
From Nature Communications: Caloric restriction improves health and survival of rhesus monkeys
 It's now 4 years being free of chronic sinusitis and off all antibiotics! Four amazing years since I (and then the rest of my family) started using easy do-it-yourself sinusitis treatments containing the probiotic (beneficial bacteria) Lactobacillus sakei. My sinuses feel great! And yes, it still feels miraculous.
It's now 4 years being free of chronic sinusitis and off all antibiotics! Four amazing years since I (and then the rest of my family) started using easy do-it-yourself sinusitis treatments containing the probiotic (beneficial bacteria) Lactobacillus sakei. My sinuses feel great! And yes, it still feels miraculous.
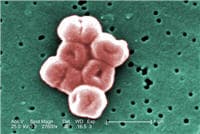 Many posts on this blog are about beneficial microbes, and the many species of microbes (bacteria, fungi, viruses) living within and on us. But there are also bacteria in the world that pose a serious threat to human health, and the list of these are growing due to antibiotic resistance. This week the World Health Organization (WHO) officials came out with a list of a dozen antibiotic-resistant "priority pathogens" that pose the greatest threats to human health. These are bacteria resistant to multiple antibiotics - thus superbugs.
Many posts on this blog are about beneficial microbes, and the many species of microbes (bacteria, fungi, viruses) living within and on us. But there are also bacteria in the world that pose a serious threat to human health, and the list of these are growing due to antibiotic resistance. This week the World Health Organization (WHO) officials came out with a list of a dozen antibiotic-resistant "priority pathogens" that pose the greatest threats to human health. These are bacteria resistant to multiple antibiotics - thus superbugs. This past week a study was published linking 8 to 10 portions of fruits and vegetables per day with a lower risk of early death, cancer, heart disease, and stroke. This confirms other research linking many daily servings of fruits and vegetables with various health benefits. For example, the study findings discussed in the
This past week a study was published linking 8 to 10 portions of fruits and vegetables per day with a lower risk of early death, cancer, heart disease, and stroke. This confirms other research linking many daily servings of fruits and vegetables with various health benefits. For example, the study findings discussed in the  Do you want to live longer and be healthy at the same time? Some possible ways may be to restrict the calories in the diet (every day) or to practice intermittent calorie restriction (a fasting mimicking diet a few days a month or even each week, such as
Do you want to live longer and be healthy at the same time? Some possible ways may be to restrict the calories in the diet (every day) or to practice intermittent calorie restriction (a fasting mimicking diet a few days a month or even each week, such as  A recent study had great results in preventing glaucoma or stopping the progress of glaucoma by supplementing the diet of mice with vitamin B3 (nicotinamide). But now the research needs to see if this also holds true for humans.
A recent study had great results in preventing glaucoma or stopping the progress of glaucoma by supplementing the diet of mice with vitamin B3 (nicotinamide). But now the research needs to see if this also holds true for humans. A new study has summarized what we know about fungi that live in and on babies - and yes, we all have fungi both on and within us. It's called the mycobiome. In healthy individuals all the microbes (bacteria, viruses, fungi, etc) live in balanced microbial communities, but the communities can become "out of whack" (dysbiosis) for various reasons, and microbes that formerly co-existed peacefully can multiply and become problematic. Or other pathogenic microbes can enter the community, and the person becomes ill.
A new study has summarized what we know about fungi that live in and on babies - and yes, we all have fungi both on and within us. It's called the mycobiome. In healthy individuals all the microbes (bacteria, viruses, fungi, etc) live in balanced microbial communities, but the communities can become "out of whack" (dysbiosis) for various reasons, and microbes that formerly co-existed peacefully can multiply and become problematic. Or other pathogenic microbes can enter the community, and the person becomes ill. A new study found differences in gut microbes between active women (they exercised at least the recommended amount) and those that are sedentary. When the gut bacteria were analyzed with modern tests (genetic sequencing) the active women had more of the health promoting beneficial bacteria such as Faecalibacterium prausnitzii, Roseburia hominis, and Akkermansia muciniphila than the sedentary women. The
A new study found differences in gut microbes between active women (they exercised at least the recommended amount) and those that are sedentary. When the gut bacteria were analyzed with modern tests (genetic sequencing) the active women had more of the health promoting beneficial bacteria such as Faecalibacterium prausnitzii, Roseburia hominis, and Akkermansia muciniphila than the sedentary women. The  Avoid eating licorice during pregnancy? That licorice is a food to avoid during pregnancy (or only eat in tiny amounts) will be news to many. Most people think of licorice (or liquorice) as a candy, but it can also be used as a herbal medicine that can have negative health effects, especially in large doses (e.g, high blood pressure, loss of potassium). The licorice flavor comes from the root of the plant (licorice root). Licorice contains glycyrrhizin, which is in black licorice candy, and in some chewing gums, ice creams, syrups, soft drinks, supplements, herbal teas, and other products.
Avoid eating licorice during pregnancy? That licorice is a food to avoid during pregnancy (or only eat in tiny amounts) will be news to many. Most people think of licorice (or liquorice) as a candy, but it can also be used as a herbal medicine that can have negative health effects, especially in large doses (e.g, high blood pressure, loss of potassium). The licorice flavor comes from the root of the plant (licorice root). Licorice contains glycyrrhizin, which is in black licorice candy, and in some chewing gums, ice creams, syrups, soft drinks, supplements, herbal teas, and other products.