 The finding that the oral bacteria Streptococcus mutans, which is found in 10% of the population, is linked with hemorrhagic strokes is big. S. mutans is found in tooth decay or cavities (dental caries). The researchers found a link with cnm-positive S. mutans with both intracerebral hemorrhage (ICH) and also with cerebral microbleeds.
The finding that the oral bacteria Streptococcus mutans, which is found in 10% of the population, is linked with hemorrhagic strokes is big. S. mutans is found in tooth decay or cavities (dental caries). The researchers found a link with cnm-positive S. mutans with both intracerebral hemorrhage (ICH) and also with cerebral microbleeds.
Some risk factors for strokes have long since been known, such as high blood pressure and advanced age, but then there are those hemorrhagic strikes that don't seem to fit the norm, with no apparent risk factors. Well, apparently the presence of cnm-positive S. mutans is one. My understanding of what cnm-positive S. mutans means is S. mutans bacteria that carries the collagen-binding Cnm gene. This bacteria can be found in a person's saliva and in dental plaque, and swabs of both were taken for this study.
This study builds on other studies that find a link between the bacteria Streptococcus mutans and a number of systemic diseases, including bacteremia, infective endocarditis and hemorrhagic stroke. The researchers of this latest study suggest that infection with cnm-positive S. mutans causes constant inflammation (as shown by 2 inflammatory markers: CRP and fibrinogen), which then causes damage to blood vessels (endothelial damage) in the brain. Bottom line: take care of your teeth and gums.
From Science Daily: Oral bacteria linked to risk of stroke
In a study of patients entering the hospital for acute stroke, researchers have increased their understanding of an association between certain types of stroke and the presence of the oral bacteria (cnm-positive Streptococcus mutans).
In the single hospital study, researchers at the National Cerebral and Cardiovascular Center in Osaka, Japan, observed stroke patients to gain a better understanding of the relationship between hemorrhagic stroke and oral bacteria. Among the patients who experienced intracerebral hemorrhage (ICH), 26 percent were found to have a specific bacterium in their saliva, cnm-positive S. mutans. Among patients with other types of stroke, only 6 percent tested positive for the bacterium.
Strokes are characterized as either ischemic strokes, which involve a blockage of one or more blood vessels supplying the brain, or hemorrhagic strokes, in which blood vessels in the brain rupture, causing bleeding.
The researchers also evaluated MRIs of study subjects for the presence of cerebral microbleeds (CMB), small brain hemorrhages which may cause dementia and also often underlie ICH. They found that the number of CMBs was significantly higher in subjects with cnm-positive S. mutans than in those without. The authors hypothesize that the S. mutans bacteria may bind to blood vessels weakened by age and high blood pressure, causing arterial ruptures in the brain, leading to small or large hemorrhages.
"This study shows that oral health is important for brain health. People need to take care of their teeth because it is good for their brain and their heart as well as their teeth," Friedland said. "The study and related work in our labs have shown that oral bacteria are involved in several kinds of stroke, including brain hemorrhages and strokes that lead to dementia."
Multiple research studies have shown a close association between the presence of gum disease and heart disease, and a 2013 publication by Jan Potempa, Ph.D., D.Sc., of the UofL School of Dentistry, revealed how the bacterium responsible for gum disease worsens rheumatoid arthritis. The cnm-negative S. mutans bacteria is found in approximately 10 percent of the general population, Friedland says, and is known to cause dental cavities (tooth decay). Friedland also is researching the role of oral bacteria in other diseases affecting the brain. http://www.nature.com/articles/srep20074

 Remember all the medical advice for years about not eating eggs frequently (high cholesterol! heart disease!) and to instead eat egg white omelettes if one absolutely wanted to eat eggs? Remember the obsession with dietary cholesterol? Well, this recent research followed 1032 men for 21 years and found that a relatively high intake of dietary cholesterol, or eating one egg every day, was not associated with an elevated risk of incident coronary heart disease - not in the entire study population nor in those with the APOE4 phenotype. Also, the study did not establish a link between dietary cholesterol or eating eggs with thickening of the common carotid artery walls. Time to enjoy eggs again! From Science Daily:
Remember all the medical advice for years about not eating eggs frequently (high cholesterol! heart disease!) and to instead eat egg white omelettes if one absolutely wanted to eat eggs? Remember the obsession with dietary cholesterol? Well, this recent research followed 1032 men for 21 years and found that a relatively high intake of dietary cholesterol, or eating one egg every day, was not associated with an elevated risk of incident coronary heart disease - not in the entire study population nor in those with the APOE4 phenotype. Also, the study did not establish a link between dietary cholesterol or eating eggs with thickening of the common carotid artery walls. Time to enjoy eggs again! From Science Daily: Another famous long-running study (Framingham Heart Study) finds more bad news for middle-aged coach-potatoes (that is, those who don't exercise or have poor physical fitness). It's an observational study (thus they found an association), but the finding is pretty damn convincing: that poor physical fitness (basically a sedentary life-style) may be linked to a smaller brain size (brain volume) 20 years later. The reason this is significant is because shrinking brain volume means that accelerated brain aging is occurring.
Another famous long-running study (Framingham Heart Study) finds more bad news for middle-aged coach-potatoes (that is, those who don't exercise or have poor physical fitness). It's an observational study (thus they found an association), but the finding is pretty damn convincing: that poor physical fitness (basically a sedentary life-style) may be linked to a smaller brain size (brain volume) 20 years later. The reason this is significant is because shrinking brain volume means that accelerated brain aging is occurring. The following is an excellent commentary by Dr. John Mandrola regarding an important British Medical Journal article that I posted about earlier (see
The following is an excellent commentary by Dr. John Mandrola regarding an important British Medical Journal article that I posted about earlier (see 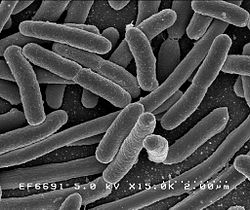 A recent study has examined the issue of whether the 10 to 1 ratio of bacteria to human cells, which is widely quoted, is actually correct. Weizmann Institute of Science researchers currently feel that based on scientific evidence (which of course will change over time) and making "educated estimates", the actual ratio is closer to 1:1 (but overall there still are more bacterial than human cells). They point out that the 10:1 ratio was originally a "back of the envelope" estimate dating back to 1972.
A recent study has examined the issue of whether the 10 to 1 ratio of bacteria to human cells, which is widely quoted, is actually correct. Weizmann Institute of Science researchers currently feel that based on scientific evidence (which of course will change over time) and making "educated estimates", the actual ratio is closer to 1:1 (but overall there still are more bacterial than human cells). They point out that the 10:1 ratio was originally a "back of the envelope" estimate dating back to 1972. Now and then I hear people wondering whether the many hours we spend staring at computer, cell phone, and tablet screens is damaging our eyes. And what about fluorescent lighting (which seems to bother many people) and LED lights? After all, the blue light of all our device screens seems intense, and researchers have long known that blue light is toxic to the retina.
Now and then I hear people wondering whether the many hours we spend staring at computer, cell phone, and tablet screens is damaging our eyes. And what about fluorescent lighting (which seems to bother many people) and LED lights? After all, the blue light of all our device screens seems intense, and researchers have long known that blue light is toxic to the retina. This study is noteworthy and relevant to humans (it was done on mice) because it may explain why so many people taking antibiotics get frequent viruses or seem more susceptible to infections. Once bacteria (both good and bad) are killed by antibiotics, then the community becomes unbalanced (dysbiosis), so that viruses may gain a foothold and a viral infection develops. In a healthy microbial community all sorts of microbes can be found, even ones we typically consider pathogenic, but the whole community keeps them in balance. One can say that "depletion of commensal microbiota also affects antiviral immunity".
This study is noteworthy and relevant to humans (it was done on mice) because it may explain why so many people taking antibiotics get frequent viruses or seem more susceptible to infections. Once bacteria (both good and bad) are killed by antibiotics, then the community becomes unbalanced (dysbiosis), so that viruses may gain a foothold and a viral infection develops. In a healthy microbial community all sorts of microbes can be found, even ones we typically consider pathogenic, but the whole community keeps them in balance. One can say that "depletion of commensal microbiota also affects antiviral immunity". Once again, research shows that "BPA-free" plastic does not mean it is safer than BPA plastic. Both BPA and BPS (the usual replacement for BPA) leach estrogenic chemicals into the foods and beverages, which means negative health effects when ingested. Both BPA and BPS mimic the effects of estrogen, as well as the actions of thyroid hormone. Yes, this study was done on zebrafish, but think of them as "the canaries in the mine" - if it affects them, it could affect humans also, especially developing fetuses and young children.
Once again, research shows that "BPA-free" plastic does not mean it is safer than BPA plastic. Both BPA and BPS (the usual replacement for BPA) leach estrogenic chemicals into the foods and beverages, which means negative health effects when ingested. Both BPA and BPS mimic the effects of estrogen, as well as the actions of thyroid hormone. Yes, this study was done on zebrafish, but think of them as "the canaries in the mine" - if it affects them, it could affect humans also, especially developing fetuses and young children.