The following medical article (actually an interview with Prof. Cedric F Garland, Department of Family & Preventive Medicine, University of California San Diego School of Medicine) is strongly in favor of Americans getting their Vitamin D levels tested, and taking vitamin D3 (if needed) to raise serum levels of vitamin D's metabolite 25(OH)D to at least 30 ng/mL and preferably more.
It is suggested that taking 1000 IU of vitamin D3 daily would achieve these levels in most people. From Medscape:
Vitamin D and Mortality Risk: Should Clinical Practice Change?
Traditionally associated with skeletal disease including osteoporosis and fractures, low levels of serum 25-hydroxyvitamin D (25[OH]D), the metabolite usually measured as a mark of vitamin D status, more recently have been linked to a wide range of nonskeletal diseases, including some cancers and autoimmune, cardiometabolic, and neurologic diseases. A number of studies also have reported an inverse association between 25(OH)D concentration and all-cause mortality.
To explore this association more, Medscape reached out to Dr. Cedric Garland, a well-known expert on vitamin D. Dr. Garland is a professor in the Division of Epidemiology, Department of Family and Preventive Medicine, and a Fellow of the American College of Epidemiology. He has a Doctor of Public Health degree from University of California San Diego and studied epidemiology at Johns Hopkins. His research has focused on vitamin D status in health and the association between vitamin D deficiency and increased risk for disease, including some common cancers (breast cancer, colon cancer, leukemia, and melanoma) and diabetes. He is active in seeking to reduce the risk for cancer and diabetes by improving vitamin D status among the US population.
To examine the relation between serum 25(OH)D and mortality, Dr. Garland and colleagues at the University of California San Diego and others in the United States pooled data from 32 studies published between 1966 and 2013.[6] They found an overall relative risk of 1.8 (95% confidence interval [CI]: 1.7-1.8; P <.001) comparing the lowest (0-9 ng/mL) with the highest (>30 ng/mL) category of 25(OH)D for all-cause mortality. Serum 25(OH)D concentrations ≤30 ng/mL were associated with higher all-cause mortality than concentrations >30 ng/mL (P <.01).
The investigators noted that these findings confirmed observations from the Institute of Medicine (IOM) that 25(OH)D levels of <20 ng/mL are too low for safety,[8] but they suggested a cut-off point of >30 ng/mL rather than >20 ng/mL for all-cause mortality reduction. This level "could be achieved in most individuals by intake of 1000 IU per day of vitamin D3," the investigators said, noting that this is described as a safe dose in almost all adults by both the IOM[8] and Endocrine Society[9] clinical guidelines on dietary intake of vitamin D.
In particular, a randomized clinical trial by Lappe et al[12] had demonstrated a reduced risk for all cancers with vitamin D supplementation in postmenopausal women.... Only one third of the US population is below 20 ng/mL,[15] but two thirds of the population is below 30 ng/mL.[16]
We decided to look at what would happen if we put together all the existing studies that have looked at the survival of "ordinary" people; that is, mostly people in general practices who did not, for the most part, have illnesses. Studies that only included people who were already ill were not eligible for inclusion in our analysis. We found 88 relevant studies, of which 32 presented their data by quartiles of intake, allowing us to see a dose response
The incidence of colon cancer is very high in countries like Iceland and Sweden, and other countries nearer the North Pole, and in countries like New Zealand, which is closer to the South Pole, and intermediate in countries at intermediate latitudes such as the United States, which is, on average, 38º north of the Equator. By the time you get down within the tropics, which is 23º from the Equator, it begins to decrease, and within 5º of the Equator there are vanishingly low incidence rates of colon cancer. In the past, some scientists theorized that the low incidence rates near the equator were due to intake of a high-fiber diet, but now my group believes -- and many others are leaning more in this direction -- that it is the high UVB irradiance and high circulating 25(OH)D year-around nearer the equator rather than a high-fiber diet that best explains the inverse association with solar UVB irradiance
Raising the serum 25(OH)D from 30 to 40 ng/mL reduces the incidence of breast, bowel, and lung cancer by 80%, as reported by Lappe and colleagues in their clinical trial.[12]On the other hand, if you lump all cancers together, in both sexes, and include countries where there is a whole lot of cigarette smoking, then you may obscure the effect of the vitamin D. Vitamin D is not able to overcome the effect of heavy smoking, and the CHANCES analysis[7] included data from people in countries like the Czech Republic, Poland, and Lithuania, where there is a huge amount of smoking. Although the effects are still there, they are weakened.
Studies such as our meta-analysis have provided us an opportunity to not just be locked into the present but to predict mortality on the basis of vitamin D levels in the present. I had expected our results to be convincing, but we were shocked at the persistence of the belief that very low levels of vitamin D, such as approximately 20 ng/mL, are safe. They are not safe with regard to breast and colon cancer, several other cancers, diabetes in youth and adulthood, fractures, and other complications of 25(OH)D <30 ng/mL. Even higher levels, such as 40-60 ng/mL, would be even safer, according to a letter of consensus of expert vitamin D scientists and physicians.
In addition, 2 ongoing trials, the CAPS study[23] (aiming to replicate the findings of Lappe et al[12]) and the VITAL study,[22] are both using a vitamin D3 dose of 2000 international units (IU)/day. I think that if I were to design a trial, knowing what we know today, I would use 4000-5000 IU/day. It seems as though each time we do a clinical trial, by the time the trial is completed, we know that the doses were too small to elicit an effect.
I am also concerned that there may be not enough calcium to see an effect. In CAPS, the women are being given 1500 mg of calcium, which was done in the original randomized controlled trial in which 80% of the cancers in postmenopausal women were prevented. I would have stayed with this design and dose for the VITAL trial. We know that it helps because in their original trial, Lappe and colleagues[12]examined the effects of vitamin D alone vs vitamin D plus calcium, and the effects were stronger when the calcium was included.
Testing should be universal. And ideally it should be done in March when the vitamin D is at its lowest levels. This will prevent hundreds of thousands of cases of serious diseases worldwide annually, beginning with postmenopausal breast cancer and including colon cancer and types 1 and 2 diabetes. Skipping this test would be equivalent to not measuring blood pressure, serum lipids, or weight at an annual exam.
No one should run a serum 25(OH)D less than 30 ng/mL. This means that two thirds of the US population needs supplementation. You may have noticed that President Obama was recently tested for his vitamin D, and it was 22.9 ng/mL.[35] His physicians wisely decided to treat him, and he is now taking vitamin D.

 Another study finding health benefits from eating dairy foods (vs not eating any dairy foods).
Another study finding health benefits from eating dairy foods (vs not eating any dairy foods).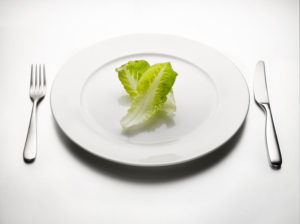 I have seen a lot of excitement about this research, especially whether several day fasting would be beneficial for other diseases (e.g., Crohn's disease) or even for middle-aged or older people who just want to boost their immune system. From Science Daily:
I have seen a lot of excitement about this research, especially whether several day fasting would be beneficial for other diseases (e.g., Crohn's disease) or even for middle-aged or older people who just want to boost their immune system. From Science Daily: Very interesting. Gives people a way to eat red meat, but not increase their colorectal cancer risk (by also eating resistant starch, e.g., potato salad or beans). From Science Daily:
Very interesting. Gives people a way to eat red meat, but not increase their colorectal cancer risk (by also eating resistant starch, e.g., potato salad or beans). From Science Daily: