 Surprising results (to me at least) from research comparing various diets and incidence of several cancers in 11,082 individuals in the Netherlands over a 20 year period. I expected the daily meat eaters to have higher rates of the 3 cancers studied, but no....
Surprising results (to me at least) from research comparing various diets and incidence of several cancers in 11,082 individuals in the Netherlands over a 20 year period. I expected the daily meat eaters to have higher rates of the 3 cancers studied, but no....
According to this study, looks like frequent meat consumption is OK when looking at lung, postmenopausal breast, and prostate cancer. Meat consumption did not increase the risk for these cancers.
Their main conclusion: vegetarians, pescatarians (eats fish, but no meat), and low-meat consumers did not have a reduced risk of lung, postmenopausal breast, and overall prostate cancer when compared with individuals consuming meat on a daily basis. This is after taking confounders such as smoking into account (because smokers have higher rates of cancers such as lung cancer).
The researchers do point out that some other similar studies had mixed results, but that perhaps those studies did not take confounders (variables that distort the results) such as smoking, physical activity levels, alcohol consumption, etc. into account.
From the European Journal of Clinical Nutrition: Vegetarianism, low meat consumption and the risk of lung, postmenopausal breast and prostate cancer in a population-based cohort study
The few prospective studies that examined lung, female breast and prostate cancer risk in vegetarians have yielded mixed results, whereas none have studied the effects of low meat diets. ... The Netherlands Cohort Study—Meat Investigation Cohort (NLCS-MIC)— is an analytical cohort of 11,082 individuals including 1133 self-reported vegetarians (aged 55–69 years at baseline). At baseline (1986), subjects completed a questionnaire on dietary habits and other risk factors for cancer and were classified into vegetarians (n=691), pescetarians (n=389), 1 day per week (n=1388), 2–5 days per week (n=2965) and 6–7 days per week meat consumers (n=5649).
After 20.3 years of follow-up, 279 lung, 312 postmenopausal breast and 399 prostate cancer cases (including 136 advanced) were available for analyses. After adjustment for confounding variables, we found no statistically significant association between meat consumption groups and the risk of lung cancer. As well, no significant associations were observed for postmenopausal breast and overall prostate cancer. After adjustment for confounders, individuals consuming meat 1 day per week were at a 75% increased risk of advanced prostate cancer compared with 6–7 days per week meat consumers.
Vegetarians, pescetarians and 1 day per week meat consumers did not have a reduced risk of lung, postmenopausal breast and overall prostate cancer compared with individuals consuming meat on a daily basis after taking confounders into account.
Although vegetarian diets are primarily defined by the absence of meat and fish, they are also shown to be associated with high intakes of fruits and vegetables and a favorable distribution of non-dietary factors.1, 2 Consequently, vegetarian diets may reduce the risk of different types of cancers through multiple mechanisms, depending on the etiology and preventability of the tumor.3, 4
We previously reported a nonsignificantly reduced risk of vegetarian and low meat diets on colorectal, and especially rectal, cancer5 and set out to study its effect on three other major cancers.
Although meat consumption has been hypothesized to be implicated in the etiology of lung, female breast and prostate cancer, data are not consistent across studies and meat subtypes.6, 7, 8However, on the basis of the existing body of literature, vegetarians may be at a lower risk of developing lung cancer (because of lower smoking rates) and to postmenopausal breast cancer (because of lower alcohol consumption, lower body mass index and higher physical activity levels).
Results from this prospective cohort study showed that, in age- and sex-adjusted models, vegetarians and pescetarians were at a reduced risk of lung cancer compared with individuals consuming meat on a daily basis. This effect disappeared after taking confounders, especially smoking, into account. We did not observe an association between the meat consumption group and the risk of post-menopausal breast and overall prostate cancer.
Our null findings regarding post-menopausal breast cancer risk are in line with other prospective studies comparing vegetarians with non-vegetarians and a pooled analysis of five cohort studies on breast cancer mortality. In contrast, the UK Women’s Cohort Study reported a lower post-menopausal breast cancer risk among non-meat consumers compared with high meat consumers,14 although this was not observed in their dietary pattern analyses.15 Vegetarian diets are rich in fiber and soy. Fiber was associated with a reduced risk of breast cancer in a meta-analysis of prospective studies,19 and soy contains isoflavones, which have previously been associated with a significant reduced risk of postmenopausal breast cancer in Asian populations.20 However, compared with the average soy intake in four Asian countries (ranging from 38 to 134 g/day21), the soy product intake among vegetarians in our population was likely too low to exert an effect (~15 g per day).
 A recent study reports more good news about eating a plant-based diet - that is, one rich in fruits, vegetables, whole grains, nuts, legumes, seeds, but low in meat and dairy foods.
A recent study reports more good news about eating a plant-based diet - that is, one rich in fruits, vegetables, whole grains, nuts, legumes, seeds, but low in meat and dairy foods.
 A recent large Swedish
A recent large Swedish  Eating your fruits and vegetables, especially a rainbow assortment of them, is associated with a lower risk of prostate cancer as well speeding up recovery in men who received radiation treatment for prostate cancer.
Eating your fruits and vegetables, especially a rainbow assortment of them, is associated with a lower risk of prostate cancer as well speeding up recovery in men who received radiation treatment for prostate cancer. Are human papilloma viruses (HPV) causing some prostate cancers? And could getting the HPV vaccine help in preventing some cases of prostate cancer? Sure sounds like it according to a recent
Are human papilloma viruses (HPV) causing some prostate cancers? And could getting the HPV vaccine help in preventing some cases of prostate cancer? Sure sounds like it according to a recent 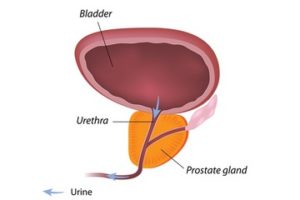
 Another reason exercise is good for you: A
Another reason exercise is good for you: A  This is a thought-provoking study that looked at environmental quality and cancer incidence in counties throughout the US. The researchers found that the more polluted the county, the higher the cancer incidence. An
This is a thought-provoking study that looked at environmental quality and cancer incidence in counties throughout the US. The researchers found that the more polluted the county, the higher the cancer incidence. An  Surprising results (to me at least) from research comparing various diets and incidence of several cancers in 11,082 individuals in the Netherlands over a 20 year period. I expected the daily meat eaters to have higher rates of the 3 cancers studied, but no....
Surprising results (to me at least) from research comparing various diets and incidence of several cancers in 11,082 individuals in the Netherlands over a 20 year period. I expected the daily meat eaters to have higher rates of the 3 cancers studied, but no....