 One study points out the difficulty of weight loss in overweight adults, because so few actually are able to get down to a normal weight or even lose a mere 5% of body weight (for example. 10 pounds for a 200 pound person or 15 pounds for a 300 pound person). The annual chance of an obese person attaining normal body weight is only 1 in 210 for men and 1 in 124 for women,and the annual chance of obese patients achieving five per cent weight loss was 1 in 12 for men and 1 in 10 for women. The second study highlights how well weight loss treats "fatty liver" (which is a problem in middle-aged overweight people). Fatty liver or nonalcoholic steatohepatitis (NASH), which affects 2 to 5 percent of Americans, can be severe and can lead to cirrhosis, in which the liver is permanently damaged and scarred and no longer able to work properly.
One study points out the difficulty of weight loss in overweight adults, because so few actually are able to get down to a normal weight or even lose a mere 5% of body weight (for example. 10 pounds for a 200 pound person or 15 pounds for a 300 pound person). The annual chance of an obese person attaining normal body weight is only 1 in 210 for men and 1 in 124 for women,and the annual chance of obese patients achieving five per cent weight loss was 1 in 12 for men and 1 in 10 for women. The second study highlights how well weight loss treats "fatty liver" (which is a problem in middle-aged overweight people). Fatty liver or nonalcoholic steatohepatitis (NASH), which affects 2 to 5 percent of Americans, can be severe and can lead to cirrhosis, in which the liver is permanently damaged and scarred and no longer able to work properly.
After reading scientific studies nonstop for the last few years, it seems that the best, easiest way to lose weight is to have lifestyle changes rather than focusing just on a "weight-loss diet": increase activity levels (yes, walking counts) and switch to a more plant based diet or Mediterranean diet (lots of fruits, vegetables, whole grains, legumes, seeds, nuts, olive oil, some fish each week) and decrease the amount of typical Western style diet (highly processed foods. lots of meat and coldcuts, lots of fat, fast foods, soda). Try to only eat within 12 hours each day (for example, 8am to 8pm) and don't eat the other 12 hours. And of course eat fewer calories (it should be easier to do if you substitute fruits and vegetables for high calorie processed foods such as ice cream, french fries, and sweets). And yes, of course it's really hard to lose weight, but the health benefits of weight loss are enormous. From Medical Xpress:
Low chance of recovering normal body weight highlights need for obesity prevention
The chance of an obese person attaining normal body weight is 1 in 210 for men and 1 in 124 for women, increasing to 1 in 1,290 for men and 1 in 677 for women with severe obesity, according to a study of UK health records led by King's College London. The findings, published in the American Journal of Public Health, suggest that current weight management programmes focused on dieting and exercise are not effective in tackling obesity at population level.The research, funded by the National Institute for Health Research (NIHR), tracked the weight of 278,982 participants (129,194 men and 149,788) women using electronic health records from 2004 to 2014.
The annual chance of obese patients achieving five per cent weight loss was 1 in 12 for men and 1 in 10 for women. For those people who achieved five per cent weight loss, 53 per cent regained this weight within two years and 78 percent had regained the weight within five years.
Overall, only 1,283 men and 2,245 women with a BMI of 30-35 reached their normal body weight, equivalent to an annual probability of 1 in 210 for men and 1 in 124 for women; for those with a BMI above 40, the odds increased to 1 in 1,290 for men and 1 in 677 for women with severe obesity. Weight cycling, with both increases and decreases in body weight, was also observed in more than a third of patients. The study concludes that current obesity treatments are failing to achieve sustained weight loss for the majority of obese patients.
Dr Alison Fildes, first author from the Division of Health and Social Care Research at King's College London (and now based at UCL), said: 'Losing 5 to 10 per cent of your body weight has been shown to have meaningful health benefits and is often recommended as a weight loss target..... More importantly, priority needs to be placed on preventing weight gain in the first place.'
From Medical Xpress: Weight loss for a healthy liver
Weight loss through both lifestyle modification and bariatric surgery can significantly reduce features of nonalcoholic steatohepatitis (NASH), a disease characterized by fat in the liver, according to two new studies published in Gastroenterology..."we most commonly see this condition in patients who are middle-aged and overweight or obese," said Giulio Marchesini, MD, from University of Bologna, Italy, and lead author of an editorial summarizing these two studies. "These two large prospective cohort studies strengthen the evidence that, no matter how you lose weight, weight loss improves liver health. Both bariatric surgery for morbidly obese patients or lifestyle modifications are viable options."
Lifestyle modifications: Eduardo Vilar-Gomez and colleagues from Cuba report in Gastroenterology that a weight reduction of 10 percent or more, induced by a comprehensive lifestyle program, is necessary to bring about NASH resolution and reverse scarring of the liver in overweight and obese patients. To a lesser degree, modest weight loss (7 to 10 percent) reduced disease severity in certain subsets of patients, including male patients and those without diabetes. Conversely, 93 percent of the patients with little or no weight reduction (less than 5 percent) experienced worsening of liver scarring....While promising, less than 50 percent of patients achieved the necessary weight loss goal of 7 to 10 percent, providing a stark reminder of the sustainability of weight loss interventions.
Bariatric surgery: For appropriate morbidly obese patients with NASH who have previously failed to lose weight through lifestyle modifications, bariatric surgery may be considered. In the second Gastroenterology study, Guillaume Lassailly and colleagues from France report that, one year after bariatric surgery, NASH had disappeared from 85 percent of patients and reduced the pathologic features of the disease after 1 year of follow-up. NASH disappeared from a higher proportion of patients with mild NASH before surgery (94 percent) than severe NASH (70 percent). More studies are needed to determine the long-term effects of bariatric surgeryin morbidly or severely obese patients with NASH.
 There is another great reason to try to lose weight if you are overweight or obese - being overweight or obese lowers blood flow to the brain in older adults. Yikes! However, one bit of good news from a study of 495 adults (average age 69) was that increased physical activity (brisk walks count!) can reduce or eliminate this association.
There is another great reason to try to lose weight if you are overweight or obese - being overweight or obese lowers blood flow to the brain in older adults. Yikes! However, one bit of good news from a study of 495 adults (average age 69) was that increased physical activity (brisk walks count!) can reduce or eliminate this association. The study found that higher levels of physical activity can reduce or remove this association of overweight & obesity and reduced brain blood flow. So if it's not possible to lose weight - then get really physically active!
The study found that higher levels of physical activity can reduce or remove this association of overweight & obesity and reduced brain blood flow. So if it's not possible to lose weight - then get really physically active!
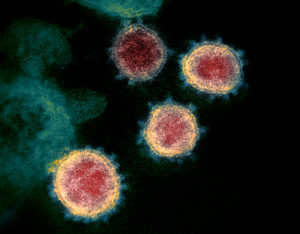 Two big risk factors are emerging over who will develop severe COVID-19 infections that lead to hospitalizations and needing intensive care. A number of studies throughout the world are reporting that the main risk factor in persons under 60 years is being significantly overweight, especially obesity, and the other risk factor is being over 65 years of age.
Two big risk factors are emerging over who will develop severe COVID-19 infections that lead to hospitalizations and needing intensive care. A number of studies throughout the world are reporting that the main risk factor in persons under 60 years is being significantly overweight, especially obesity, and the other risk factor is being over 65 years of age.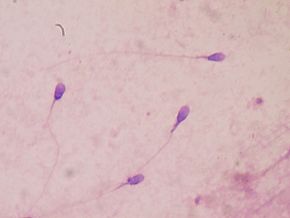 Another problem for overweight or obese men: an increased risk of poor sperm quality.
Another problem for overweight or obese men: an increased risk of poor sperm quality.  Yup, according to a new mega-study, being overweight or obese is linked to higher risk of dying prematurely than being normal weight. And the more you weigh, the greater the risk.
Yup, according to a new mega-study, being overweight or obese is linked to higher risk of dying prematurely than being normal weight. And the more you weigh, the greater the risk.  Obesity rates in the US are high! Obesity rates in the US were 35% among men and 40.4% in women in 2013-2014, and extreme obesity (class 3) rates were 5.5% for men and 9.9% for women. Obesity is defined as a body mass index (BMI) 30 or greater (≥30), and extreme obesity or class 3 obesity is a body mass index of 40 or greater (BMI ≥40).
Obesity rates in the US are high! Obesity rates in the US were 35% among men and 40.4% in women in 2013-2014, and extreme obesity (class 3) rates were 5.5% for men and 9.9% for women. Obesity is defined as a body mass index (BMI) 30 or greater (≥30), and extreme obesity or class 3 obesity is a body mass index of 40 or greater (BMI ≥40). A report released this week by the Endocrine Society states that the list of health problems that scientists can confidently link to exposure to hormone-disrupting chemicals has grown to include: diabetes, cardiovascular disease, obesity, reproductive and developmental problems, thyroid impairment, certain reproductive cancers, and neurodevelopmental problems such as decreased IQ. This statement (report) is based on the summaries of 1300 studies on endocrine disrupting chemicals (EDCs), and it also adds support to the idea that even
A report released this week by the Endocrine Society states that the list of health problems that scientists can confidently link to exposure to hormone-disrupting chemicals has grown to include: diabetes, cardiovascular disease, obesity, reproductive and developmental problems, thyroid impairment, certain reproductive cancers, and neurodevelopmental problems such as decreased IQ. This statement (report) is based on the summaries of 1300 studies on endocrine disrupting chemicals (EDCs), and it also adds support to the idea that even  Some recent studies looked at aspirin use and cancer and found that consistent use for a number of years (5 to 10 years) lowers the rate of a number of cancers, including colon cancer. However, the longer one takes daily aspirin - then harms start adding up, with a major one being gastrointestinal bleeding. NSAIDs (non-steroidal anti-inflammatory drugs) are also linked to lower rates of various cancers, but harms with long-term use are cardiovascular risks (stroke and heart attack). The first article discusses that many doctors think this lower cancer rate occurs because aspirin and NSAIDs
Some recent studies looked at aspirin use and cancer and found that consistent use for a number of years (5 to 10 years) lowers the rate of a number of cancers, including colon cancer. However, the longer one takes daily aspirin - then harms start adding up, with a major one being gastrointestinal bleeding. NSAIDs (non-steroidal anti-inflammatory drugs) are also linked to lower rates of various cancers, but harms with long-term use are cardiovascular risks (stroke and heart attack). The first article discusses that many doctors think this lower cancer rate occurs because aspirin and NSAIDs  One study points out the difficulty of weight loss in overweight adults, because so few actually are able to get down to a normal weight or even lose a mere 5% of body weight (for example. 10 pounds for a 200 pound person or 15 pounds for a 300 pound person). The annual chance of an
One study points out the difficulty of weight loss in overweight adults, because so few actually are able to get down to a normal weight or even lose a mere 5% of body weight (for example. 10 pounds for a 200 pound person or 15 pounds for a 300 pound person). The annual chance of an