 Many probiotic manufacturers say that their product has all sorts of wonderful health benefits in people eating that particular probiotic, but is the evidence there? Finally, now there is a review of the best existing studies looking at whether probiotics have any effect on the gut bacteria of healthy, normal individuals. In other words, are the probiotics even staying there (to have some beneficial effect) or do they just "pass through" without leaving anything behind?
Many probiotic manufacturers say that their product has all sorts of wonderful health benefits in people eating that particular probiotic, but is the evidence there? Finally, now there is a review of the best existing studies looking at whether probiotics have any effect on the gut bacteria of healthy, normal individuals. In other words, are the probiotics even staying there (to have some beneficial effect) or do they just "pass through" without leaving anything behind?
The main finding: only one study out of 7 found any lasting effect on gut microbes (in healthy individuals) from the probiotics which had been ingested daily over varying times, but typically for one month. Note: RCTs are randomly controlled trials, which are the best way to test whether something has an effect - because people are randomly assigned to a group. In these studies no one knew who was getting a placebo (e.g., received capsule without the probiotic) or the probiotic (e.g., in the capsule) - this eliminates self-selection and bias. But perhaps the bacteria strains tested were the wrong ones? Or the time period wasn't long enough or the bacteria weren't given in sufficient amounts? Also, studies didn't test multi-strain probiotics (which people commonly take), but only 1 or 2 species of bacteria.
However, other research has shown benefits from probiotics in individuals with "dysbiosis" (microbial communities out of whack) or certain illnesses. It'll be interesting to see what further research finds. These are still early days in this research. From MedicalXpress:
Do probiotics have an effect on healthy adults? It's too early to tell
There is little evidence to support any consistent effect of probiotics on the gut microbiota of healthy individuals, according to a systematic review published in the open access journal Genome Medicine. The World Health Organization defines probiotics as live microorganisms which confer a health benefit to the host if administered in adequate amounts and probiotics products are often marketed toward the general population. However, evidence for their effects on bacteria living in the guts of healthy adults remains elusive.
The study by researchers at the Novo Nordisk Foundation Center for Basic Metabolic Research at the University of Copenhagen is a systematic review of seven randomized controlled trials (RCTs) investigating the effect of probiotic products on the fecal microbiota of healthy adults.
Nadja Buus Kristensen, PhD student and junior author, said: "According to our systematic review, no convincing evidence exists for consistent effects of examined probiotics on fecal microbiota composition in healthy adults, despite probiotic products being consumed to a large extent by the general population."...The authors found that of the seven original RCTs included in the study, only one observed significantly greater changes in the bacterial species composition of the fecal microbiota in individuals who consumed probiotics compared to those who did not.
Also, an international consensus on what defines a normal or healthy fecal microbial community is lacking....Study participants across the seven original RCTs included in this review were healthy adults between 19 and 88 years of age. Numbers of individuals ranged from 21 to 81 and the proportion of women was between 50 and 100%. Probiotic products were administered as biscuits, milk-based drinks, sachets, or capsules for periods of 21 to 42 days.
Oluf Pedersen, professor at the University of Copenhagen and senior author of the paper said: "While there is some evidence from previous reviews that probiotic interventions may benefit those with disease-associated imbalances of the gut microbiota, there is little evidence of an effect in healthy individuals.


 This confirms what researchers such as
This confirms what researchers such as  More long-standing medical advice goes out the window. New advice: avoid diet soda and artificial sweeteners. The amazing part is that our gut bacteria are involved.
More long-standing medical advice goes out the window. New advice: avoid diet soda and artificial sweeteners. The amazing part is that our gut bacteria are involved.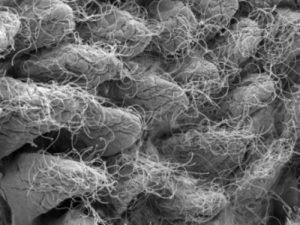 This image depicts gut microbiota.
This image depicts gut microbiota.  A big benefit to exercising - more microbial diversity, which means a healthier gut microbiome, which means better health. From Medscape:
A big benefit to exercising - more microbial diversity, which means a healthier gut microbiome, which means better health. From Medscape: