It turns out there are a number of simple things you can do to keep your sinuses healthy and reduce the chances of developing another sinus infection. A lot of these suggestions involve preventing nasal stuffiness and congestion, and to improve sinus drainage.
Because, as we all know - once those nasal passages get clogged, the odds of another sinus infection increases. When the nasal passages are inflamed or blocked, then mucus can't properly drain from the sinuses.
Chronic sinusitis goes hand in hand with rhinitis, which is why the medical literature refers to chronic sinusitis as chronic rhinosinusitis. It can be allergic rhinitis or non-allergic rhinitis - that is, with known or unknown triggers leading to a dripping nose, congestion, increased mucus, even sneezing or coughing. Dust, irritants, fragrances, allergies (e.g., tree pollen), spicy foods, and air pollution are all examples of triggers.
Some of the following tips are to avoid fragrances and scented products. This is because they are considered indoor air pollutants. They release chemicals that cause nasal inflammation, which can result in rhinitis symptoms, and possibly lead to sinusitis. All air pollution (whether indoors or outdoors) can cause nasal inflammation.
TWENTY TIPS FOR SINUS HEALTH:
1) Sleep with 2 or more pillows in a semi-upright position. This helps with mucus drainage in the nasal passages.
2) When needed, use an ordinary saline nasal rinse once or twice a day. This helps with nasal congestion.
3) When needed, use a 12-hour 1200 mg guaifenesin non-prescription product (e.g., Mucinex) at night. It helps to thin mucus.
4) Can use antihistamines (for allergies) and nasal corticosteroid sprays (especially for nasal polyps) when needed.
5) Can use a premade saline mist spray (e.g., Arm and Hammer simply saline mist) to help relieve minor congestion. This can be helpful any place with stuffy air.
6) Shower at night to wash away dust and allergens.
7) Use unscented personal care products as much as possible (e.g., unscented deodorant). Or if that's not possible, try for minimally scented products.
8) Avoid cigarette smoke and smoke-filled air as much as possible.
9) Consider limiting your intake of alcohol. Alcohol causes temporary nasal inflammation in everyone, but for some persons the swelling lasts a long time and can cause nasal congestion and other symptoms.
10) Avoid the use of scented products in the home, including air fresheners, scented candles, incense, essential oils, clothes detergents, and scented dryer sheets (fragrances/chemicals are air pollutants - in the air, get on our clothes, and us).
11) Frequently open windows to air out the home, even if only for a few minutes. Use bathroom fans if you have them.
12) When cooking, use a kitchen exhaust fan that vents to the outside, especially if you have a gas stove and oven.
13) Vacuum frequently with a good vacuum cleaner.
14) Wall to wall carpeting can be a problem for many, especially in the bedroom. They accumulate dust and contaminants, which are hard to clean.
15) Change your A/C and heating filters frequently.
16) Consider getting a good air purifier (check Consumer Reports and Wirecutter. Especially powerful are the Austin Air Purifiers.)
17) Make sure there isn't a hidden mold problem, and clean up any mold you find. Also, make sure that water isn't getting into the house. [CDC guidelines]
WHEN STARTING TO FEEL SINUSITIS SYMPTOMS:
18) Get enough sleep. When sleep deprived, people can feel “mucusy”. They are also more susceptible to viruses.
19) At the start of a sore throat or infection - suck on a zinc tablet or lozenge. It may stop the viral infection.
20) Use L. sakei (e.g., Lanto Sinus) at the start of a sinus infection. (Stop using it when feeling better.)
 Additionally, try to boost your immune system by eating a healthy diet (one rich in fruits, vegetables, whole grains, seeds, nuts, legumes, olive oil), getting plenty of sleep, drinking plenty of water, and getting enough exercise or physical activity (Government guidelines say at least 2 1/2 hours per week of physical activity, including walking).
Additionally, try to boost your immune system by eating a healthy diet (one rich in fruits, vegetables, whole grains, seeds, nuts, legumes, olive oil), getting plenty of sleep, drinking plenty of water, and getting enough exercise or physical activity (Government guidelines say at least 2 1/2 hours per week of physical activity, including walking).
Can also take a vitamin D supplement (research shows it can decrease the number of respiratory infections) or get enough sunlight. After all, vitamin D is called the sunshine vitamin.
Good health!

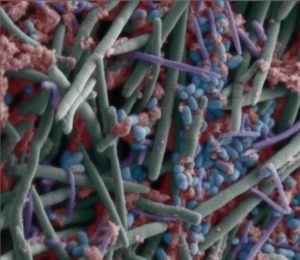

 Some microbes have an important role in the health of the sinus microbiome, even if they are there only in tiny amounts – these are keystone bacteria. Lactobacillus sakei is one of them (in
Some microbes have an important role in the health of the sinus microbiome, even if they are there only in tiny amounts – these are keystone bacteria. Lactobacillus sakei is one of them (in