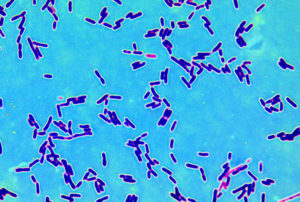
 Could probiotics be used to treat depression? The medical site Medscape reported on a very small preliminary study (only 10 people) that tested that idea, with findings that suggested that taking certain probiotics does help treat the symptoms of mild to moderate depression. The bacteria taken were Lactobacillus helveticus and Bifidobacterium longum (in the product Probio'Stick). Specifically, the symptoms of mood, anhedonia (inability to feel pleasure), and sleep disturbance were significantly reduced after probiotoc therapy.
Could probiotics be used to treat depression? The medical site Medscape reported on a very small preliminary study (only 10 people) that tested that idea, with findings that suggested that taking certain probiotics does help treat the symptoms of mild to moderate depression. The bacteria taken were Lactobacillus helveticus and Bifidobacterium longum (in the product Probio'Stick). Specifically, the symptoms of mood, anhedonia (inability to feel pleasure), and sleep disturbance were significantly reduced after probiotoc therapy.
Sounds great, yes? But ....just a few months ago a much larger study was published where people were randomly assigned to either a placebo group or the treatment group (the same 2 probiotics: Lactobacillus helveticus and Bifidobacterium longum). It was also "double-blind" - so no one knew who got the placebo or the treatment. And here the results were: the probiotics did NOT help the depression symptoms. This study found "no evidence that the probiotic formulation is effective in treating low mood, or in moderating the levels of inflammatory and other biomarkers".
Why the different results? Maybe the "placebo effect" was why the 10 person study had a positive effect. Wanting and thinking something works can definitely influence results. (This is why ideally studies are double-blind, randomized, and with a placebo.) Or was it because the study was done "in association" with the manufacturers of Probio'Stick? Yup, it's not surprising the manufacturer of a product finds a "positive effect" from its product. Bottom line: Be careful and critical when reading "study results".
However, after saying all that - there is a "gut-brain axis" in humans, and some researchers are examining whether probiotics can treat various symptoms such as anxiety (here and here). So perhaps some other probiotic bacteria might work to treat depression.
The problematic study from Medscape: Probiotics Promising for Mild to Moderate Depression
Probiotics may be effective in reducing core depressive symptoms in treatment-naive patients with a mild to moderate form of the disorder, results of a new pilot study suggest. Investigators led by Caroline Wallace, PhD candidate, Queen's University, Kingston, Ontario, Canada, found that symptoms of mood, anhedonia, and sleep disturbance were significantly reduced with probiotic therapy after just 4 weeks, with results maintained at 8 weeks..... The hypothesis is that the effects are mediated via the gut-brain axis by reducing inflammation and increasing serotonin levels.
To assess the efficacy of probiotics in treatment-naive patients with depression, the researchers carried out a pilot study using Probio'Stick, a probiotic supplement that combines two different strains known to act on the gut-brain axis ― Lactobacillus helveticus R0052 and Bifidobacterium longum R0175. The 8-week, single-arm, open-label intervention pilot study involved 10 treatment-naive patients with major depressive disorder who were experiencing a current episode of depression..... Next steps will be to confirm these findings in a double-blind, randomized, placebo-controlled trial of Probio'Stick.
Same probiotic bacteria, but no effect from the treatment. From The Australian and New Zealand Journal of Psychiatry: A double-blind, randomized, placebo-controlled trial of Lactobacillus helveticus and Bifidobacterium longum for the symptoms of depression.
No significant difference was found between the probiotic and placebo groups on any psychological outcome measure or any blood-based biomarker.
This study found no evidence that the probiotic formulation is effective in treating low mood, or in moderating the levels of inflammatory and other biomarkers. The lack of observed effect on mood symptoms may be due to the severity, chronicity or treatment resistance of the sample; recruiting an antidepressant-naive sample experiencing mild, acute symptoms of low mood, may well yield a different result. Future studies taking a preventative approach or using probiotics as an adjuvant treatment may also be more effective. Vitamin D levels should be monitored in future studies in the area. The results of this trial are preliminary; future studies in the area should not be discouraged.

 A study of 60 million Americans 65 years old and older (the entire Medicare population) found that long-term exposure to airborne fine particulate matter (PM2.5) and ozone at concentrations below current national standards increases the risk of premature death ("all cause mortality") even when the levels are below current national standards. This effect was most pronounced among racial minorities and people with low income. The national standards are called
A study of 60 million Americans 65 years old and older (the entire Medicare population) found that long-term exposure to airborne fine particulate matter (PM2.5) and ozone at concentrations below current national standards increases the risk of premature death ("all cause mortality") even when the levels are below current national standards. This effect was most pronounced among racial minorities and people with low income. The national standards are called  I'm starting to see studies questioning whether some of the beneficial health effects that many attribute to
I'm starting to see studies questioning whether some of the beneficial health effects that many attribute to  This week a forceful statement paper was issued by more than 200 hundred scientists and health professionals expressing serious concerns about triclosan and triclocarban. This statement, called
This week a forceful statement paper was issued by more than 200 hundred scientists and health professionals expressing serious concerns about triclosan and triclocarban. This statement, called  Should the results of this study determine what kind of coffee one drinks? Does it really make a difference? Eh...Not for me (because all coffee seems to be beneficial), but it might for you.
Should the results of this study determine what kind of coffee one drinks? Does it really make a difference? Eh...Not for me (because all coffee seems to be beneficial), but it might for you. Hah! A study that builds on what is already known by many women - that the non-prescription product D-mannose works for urinary tract infections (UTIs). D-mannose is amazingly effective for urinary tract infections caused by E. coli bacteria (up to 90% of UTIs), even infections that keep recurring (30 to 50% of infections), and which don't respond to numerous antibiotics.
Hah! A study that builds on what is already known by many women - that the non-prescription product D-mannose works for urinary tract infections (UTIs). D-mannose is amazingly effective for urinary tract infections caused by E. coli bacteria (up to 90% of UTIs), even infections that keep recurring (30 to 50% of infections), and which don't respond to numerous antibiotics. Everyone has heard about the miraculous stories of recovery from cancer using immunotherapy. Immunotherapy involves giving the sick person substances which stimulate the person's own immune system to battle the cancer. And when it works, it's wonderful. But...there's another side - a dark side of the harms from these treatments - that is rarely discussed, and why we should be very careful going forward.
Everyone has heard about the miraculous stories of recovery from cancer using immunotherapy. Immunotherapy involves giving the sick person substances which stimulate the person's own immune system to battle the cancer. And when it works, it's wonderful. But...there's another side - a dark side of the harms from these treatments - that is rarely discussed, and why we should be very careful going forward.