 Why is the US Department of Agriculture (USDA) dropping plans to test for glyphosate residues in food? It was supposed to start soon (April 1, 2017), in coordination with the Environmental Protection Agency (EPA) and the Food and Drug Administration (FDA), but now all plans to test have been dropped. Why is this worrisome? The issue is that glyphosate is currently the most widely used pesticide in the world. It is a herbicide that is the active ingredient in the herbicide commonly known as Roundup. Global use was 1.65 billion pounds in 2014 , while overall use in the US was 276.4 million pounds in 2014. Glyphosate is a probable human carcinogen and linked to various health effects, and research shows that glyphosate residues are commonly found in foods.
Why is the US Department of Agriculture (USDA) dropping plans to test for glyphosate residues in food? It was supposed to start soon (April 1, 2017), in coordination with the Environmental Protection Agency (EPA) and the Food and Drug Administration (FDA), but now all plans to test have been dropped. Why is this worrisome? The issue is that glyphosate is currently the most widely used pesticide in the world. It is a herbicide that is the active ingredient in the herbicide commonly known as Roundup. Global use was 1.65 billion pounds in 2014 , while overall use in the US was 276.4 million pounds in 2014. Glyphosate is a probable human carcinogen and linked to various health effects, and research shows that glyphosate residues are commonly found in foods.
Even though whether glyphosate is a carcinogen is hotly debated by some groups (with Monsanto fiercely fighting against such a label), it shouldn't matter in the decision of whether to test for glyphosate residues in foods. What is going on with our food, and whether and how much glyphosate residues are in food should be monitored. Government agencies (such as USDA) test for other pesticide residues, and they should do the same for glyphosate, especially because it is so widely used.
The FDA did test for a short while last year (2016) and then stopped in the fall, and yes, they found residues in the foods they studied. Government and private testing has already found glyphosate residues in breast milk, soybeans, corn, honey, cereal, wheat flour, oatmeal, soy sauce, beer, and infant formula. It is currently unknown what the glyphosate residues in food that we eat means for human health. Several studies have linked glyphosate to human health ailments, including non-Hodgkin lymphoma and kidney and liver problems. Of special concern is that because glyphosate is so pervasive in the environment, even trace amounts might be harmful due to chronic exposure. Glyphosate is patented by its manufacturer (Monsanto) for its antibacterial properties - thus it can be viewed as an antibiotic. What is it doing to our gut microbes when ingested? Some people (including researchers) are even suggesting that much of "gluten sensitivity" or "gluten intolerance" that people complain of, may actually be sensitivity to glyphosate residues in food. There are many unanswered questions.
So....is this a case of burying the head in the sand? That there are no problems if no one looks for them? The EPA has long known that glyphosate residues are occurring in food because in 2013 the EPA raised "tolerance limits" for human exposure to glyphosate for certain foods, stating with "reasonable certainty that no harm will result" from human exposure to the chemical. This increase in tolerance levels came about from a request from Monsanto (the manufacturer of the glyphosate herbicide Roundup), and even though numerous groups protested the increase, the EPA went along with Monsanto's request. Some tolerances doubled. Pesticide residues are an important issue - because we don't know what chronic exposure to mixtures of low levels of pesticides (which includes glyphosate) in foods does to us. To babies and children, to pregnant women, to the elderly, to all of us.
But remember.... there are very strong industry pressures on the EPA and USDA, with some government officials also having ties to the industry, and so perhaps it's a case of keeping the head firmly in the sand for all sorts of pesticide issues. Maybe the motto is: see no evil...hear no evil....There have been some lawsuits from people claiming harm from the pesticide, as well as push back from scientists and environmental groups. Some influential scientists and physicians came out with a Statement of Concern in 2016 regarding their serious concerns with glyphosate.
The reason that glyphosate tolerance limits needed to be increased in the USA is because Roundup Ready crops are now so extensively planted, and this has resulted in skyrocketing use of glyphosate in the last 20 years. Roundup Ready crops are genetically modified to tolerate repeated glyphosate spraying (against weeds) during the growing season. However, the crops take up and accumulate glyphosate, and so glyphosate residues are increasing in crops. Another reason for increased residue of glyphosate in crops is the current practice of applying an herbicide such as Roundup right at the time of harvest to non-GMO crops such as wheat, so that the crop dies at once and dries out (pre-harvest crop dessication), and which is called a "preharvest application" by Monsanto. Glyphosate is now off-patent so many other companies are also using glyphosate in their products throughout the world.
How to lower your daily intake of glyphosate? Eat organic foods as much as possible, including wheat, corn, oats, soybeans. Glyphosate is not allowed to be used in organic food production. The following excerpts are from an article by journalist Carey Gillam, and it is well worth reading the entire article. From The Huffington Post:
USDA Drops Plan to Test for Monsanto Weed Killer in Food
The U.S. Department of Agriculture has quietly dropped a plan to start testing food for residues of glyphosate, the world’s most widely used weed killer and the key ingredient in Monsanto Co.’s branded Roundup herbicides. The agency spent the last year coordinating with the Environmental Protection Agency (EPA) and the Food and Drug Administration (FDA) in preparation to start testing samples of corn syrup for glyphosate residues on April 1, according to internal agency documents obtained through Freedom of Information Act requests. Documents show that at least since January 2016 into January of this year, the glyphosate testing plan was moving forward. But when asked about the plan this week, a USDA spokesman said no glyphosate residue testing would be done at all by USDA this year.
The USDA’s plan called for the collection and testing of 315 samples of corn syrup from around the United States from April through August, according to the documents. Researchers were also supposed to test for the AMPA metabolite, the documents state. AMPA (aminomethylphosphonic acid) is created as glyphosate breaks down. Measuring residues that include those from AMPA is important because AMPA is not a benign byproduct but carries its own set of safety concerns, scientists believe.
The USDA does not routinely test for glyphosate as it does for other pesticides used in food production. But that stance has made the USDA the subject of criticism as controversy over glyphosate safety has mounted in recent years. The discussions of testing this year come as U.S. and European regulators are wrestling with cancer concerns about the chemical, and as Monsanto, which has made billions of dollars from its glyphosate-based herbicides, is being sued by hundreds of people who claim exposures to Roundup caused them or their loved ones to suffer from non-Hodgkin lymphoma. Internal Monsanto documents obtained by plaintiffs’ attorneys in those cases indicate that Monsanto may have manipulated research regulators relied on to garner favorable safety assessments, and last week, Congressman Ted Lieu called for a probe by the Department of Justice into Monsanto’s actions.
Along with the USDA, the Food and Drug Administration also annually tests thousands of food samples for pesticide residues. Both agencies have done so for decades as a means to ensure that traces of weed killers, insecticides, fungicides and other chemicals used in farming do not persist at unsafe levels in food products commonly eaten by American families. If they find residues above the “maximum residue level” (MRL) allowed for that pesticide and that food, the agencies are supposed to inform the EPA, and actions can be taken against the supplier. The EPA is the regulator charged with establishing MRLs, also called “tolerances,” for different types of pesticides in foods, and the agency coordinates with USDA and FDA on the pesticide testing programs.
But despite the fact that glyphosate use has surged in the last 20 years alongside the marketing of glyphosate-tolerant crops, both USDA and FDA have declined to test for glyphosate residues aside from one time in 2011 when the USDA tested 300 soybean samples for glyphosate and AMPA residues. At that time the agency found 271 samples contained glyphosate, but said the levels were under the MRL - low enough not to be worrisome. The Government Accountability Office took both agencies to task in 2014 for the failure to test regularly for glyphosate.
The USDA’s most recent published report on pesticide residues in food found that for 2015 testing, only 15 percent of the 10,187 samples tested were free from any detectable pesticide residues. That’s a marked difference from 2014, when the USDA found that over 41 percent of samples were “clean” or showed no detectable pesticide residues. But the agency said the important point was that most of the samples, over 99 percent, had residues below the EPA’s established tolerances and are at levels that “do not pose risk to consumers’ health and are safe.” Many scientists take issue with using MRLs as a standard associated with safety, arguing they are based on pesticide industry data and rely on flawed analyses. Much more research is needed to understand the impact on human health of chronic dietary exposures to pesticides, many say.
![]() On this Earth Day I want to say: Support science. Support the work of scientists. Science is the pursuit of knowledge. Science is about facts and evidence - not opinions. Medicine is applied science - scientific discoveries are turned into real-world medical treatments. Yes, scientific theories and what we know in science and medicine can change over time as more evidence is found. But science is not political, or it shouldn't be political. This is because we all benefit from science and scientific knowledge.
On this Earth Day I want to say: Support science. Support the work of scientists. Science is the pursuit of knowledge. Science is about facts and evidence - not opinions. Medicine is applied science - scientific discoveries are turned into real-world medical treatments. Yes, scientific theories and what we know in science and medicine can change over time as more evidence is found. But science is not political, or it shouldn't be political. This is because we all benefit from science and scientific knowledge.
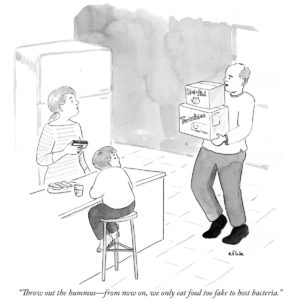

 Credit: R. Glasbergen
Credit: R. Glasbergen Sooo.....what is going on here? Why are very early onset (5 years and younger) pediatric inflammatory bowel diseases (IBD) in children increasing so rapidly in Canada? Inflammatory bowel diseases include
Sooo.....what is going on here? Why are very early onset (5 years and younger) pediatric inflammatory bowel diseases (IBD) in children increasing so rapidly in Canada? Inflammatory bowel diseases include  Huh?...A
Huh?...A  A possible problem with running marathons is short term kidney injury in the two days right after the race. A study of 22 runners in the 2015 Hartford (Connecticut) Marathon found that most of the runners temporarily developed acute kidney injury (AKI) directly after the race. The study main author Chirag R. Parikh, MD, PhD said: "The kidney responds to the physical stress of marathon running as if it's injured, in a way that's similar to what happens in hospitalized patients when the kidney is affected by medical and surgical complications".
A possible problem with running marathons is short term kidney injury in the two days right after the race. A study of 22 runners in the 2015 Hartford (Connecticut) Marathon found that most of the runners temporarily developed acute kidney injury (AKI) directly after the race. The study main author Chirag R. Parikh, MD, PhD said: "The kidney responds to the physical stress of marathon running as if it's injured, in a way that's similar to what happens in hospitalized patients when the kidney is affected by medical and surgical complications". Why is the US Department of Agriculture (USDA) dropping plans to test for glyphosate residues in food? It was supposed to start soon (April 1, 2017), in coordination with the Environmental Protection Agency (EPA) and the Food and Drug Administration (FDA), but now all plans to test have been dropped. Why is this worrisome? The issue is that glyphosate is currently the most widely used pesticide in the world. It is a herbicide that is the active ingredient in the herbicide commonly known as Roundup. Global use was 1.65 billion pounds in 2014 , while overall use in the US was 276.4 million pounds in 2014. Glyphosate is a
Why is the US Department of Agriculture (USDA) dropping plans to test for glyphosate residues in food? It was supposed to start soon (April 1, 2017), in coordination with the Environmental Protection Agency (EPA) and the Food and Drug Administration (FDA), but now all plans to test have been dropped. Why is this worrisome? The issue is that glyphosate is currently the most widely used pesticide in the world. It is a herbicide that is the active ingredient in the herbicide commonly known as Roundup. Global use was 1.65 billion pounds in 2014 , while overall use in the US was 276.4 million pounds in 2014. Glyphosate is a  Did you know that some foods have nanoparticles added to them?
Did you know that some foods have nanoparticles added to them?  Another study not finding benefits from taking supplements - this time older men taking vitamin E and selenium supplements to see if it prevents dementia and Alzheimer's disease. The men (average age 67.5 years) were randomly assigned to take either
Another study not finding benefits from taking supplements - this time older men taking vitamin E and selenium supplements to see if it prevents dementia and Alzheimer's disease. The men (average age 67.5 years) were randomly assigned to take either  A new study has been released that reminds us that all drugs (whether prescription or non-prescription) have side-effects. This time a
A new study has been released that reminds us that all drugs (whether prescription or non-prescription) have side-effects. This time a