 In the past few months there has been a lot of discussion about early screening tests for cancer (when there are no symptoms) versus diagnostic tests (testing once symptoms appear), especially for prostate cancer and breast cancer. Because unfortunately screening also has harms - it is not without significant risks. So the following 2 articles discussing breast cancer are real eye openers. The first article discusses a large study that found that no matter how early the screening and no matter how tiny the cancer and extensive the treatment (e.g, mastectomy of both breasts), in a certain percentage of women the cancer will reappear in a deadly fashion and eventually kill about 3.3% even though they are treated early. The Medscape article points out that it is thought that 28% of early stage breast cancers will progress or reappear as deadly metastatic cancer (even years later) no matter the treatment.
In the past few months there has been a lot of discussion about early screening tests for cancer (when there are no symptoms) versus diagnostic tests (testing once symptoms appear), especially for prostate cancer and breast cancer. Because unfortunately screening also has harms - it is not without significant risks. So the following 2 articles discussing breast cancer are real eye openers. The first article discusses a large study that found that no matter how early the screening and no matter how tiny the cancer and extensive the treatment (e.g, mastectomy of both breasts), in a certain percentage of women the cancer will reappear in a deadly fashion and eventually kill about 3.3% even though they are treated early. The Medscape article points out that it is thought that 28% of early stage breast cancers will progress or reappear as deadly metastatic cancer (even years later) no matter the treatment.
As Dr. Welch has pointed out in his book Overdiagnosis and Less Medicine, More Health - these aggressive cancers are like "birds" - they fly away throughout the body and are deadly no matter when they are diagnosed. A certain percentage of tiny cancers regress (disappear) on their own, others just sit there doing nothing, others grow very slowly (and can be treated successfully when symptoms appear), and then there are those that are so very aggressive that they go throughout the body from the beginning (the birds). And we don't know which will be the aggressive ones when we first find them. So sad..... Meanwhile try to eat healthy foods, get enough sleep, lose weight if overweight, live a healthy lifestyle (don't smoke or drink to excess), and get plenty of exercise in hopes of cancer prevention. I also like to think that each week eating some turmeric (in foods), broccoli famiy foods, olive oil, and berries may also help. Do go read the full original articles. From NY Times:
Early-Stage Breast Condition May Not Require Cancer Treatment
As many as 60,000 American women each year are told they have a very early stage of breast cancer — Stage 0, as it is commonly known — a possible precursor to what could be a deadly tumor. And almost every one of the women has either a lumpectomy or a mastectomy, and often a double mastectomy, removing a healthy breast as well. Yet it now appears that treatment may make no difference in their outcomes. Patients with this condition had close to the same likelihood of dying of breast cancer as women in the general population, and the few who died did so despite treatment, not for lack of it, researchers reported Thursday in JAMA Oncology.
Their conclusions were based on the most extensive collection of data ever analyzed on the condition, known as ductal carcinoma in situ, or D.C.I.S.: 100,000 women followed for 20 years. The findings are likely to fan debate about whether tens of thousands of patients are undergoing unnecessary and sometimes disfiguring treatments for premalignant conditions that are unlikely to develop into life-threatening cancers.
Diagnoses of D.C.I.S., involving abnormal cells confined to the milk ducts of the breast, have soared in recent decades. They now account for as much as a quarter of cancer diagnoses made with mammography, as radiologists find smaller and smaller lesions. But the new data on outcomes raises provocative questions: Is D.C.I.S. cancer, a precursor to the disease or just a risk factor for some women? Is there any reason for most patients with the diagnosis to receive brutal therapies? If treatment does not make a difference, should women even be told they have the condition?
A majority of the 100,000 patients in the database the researchers used, from a national cancer registry, had lumpectomies, and nearly all the rest had mastectomies, the new study found. Their chance of dying of breast cancer in the two decades after treatment was 3.3 percent, no matter which procedure they had, about the same as an average woman’s chance of dying of breast cancer, said Dr. Laura J. Esserman, a breast cancer surgeon and researcher at the University of California, San Francisco, who wrote an editorial accompanying the study.
The data showed that some patients were at higher risk: those younger than 40, black women, and those whose abnormal cells had molecular markers found in advanced cancers with poorer prognoses. D.C.I.S. has long been regarded as a precursor to potentially deadly invasive cancers, analogous to colon polyps that can turn into colon cancer, said Dr. Steven A. Narod, the lead author of the paper and a researcher at Women’s College Research Institute in Toronto. The treatment strategy has been to get rid of the tiny specks of abnormal breast cells, just as doctors get rid of colon polyps when they see them in a colonoscopy.
But if that understanding of the condition had played out as expected, women who had an entire breast removed, or even both breasts as a sort of double precaution, should have been protected from invasive breast cancer. Instead, the findings showed, they had the same risk as those who had a lumpectomy. Almost no women went untreated, so it is not clear if as a group, they did worse. But some women who died of breast cancer ended up with the disease throughout their body without ever having it recur in their breast — many, in fact, had no breast because they had had a mastectomy. Those very rare fatal cases of D.C.I.S. followed by fatal breast cancer, Dr. Narod concluded, had most likely already spread at the time of detection. As for the rest, he said, they were never going to spread anyway.
Dr. Esserman said that if deadly breast cancers started out as D.C.I.S., the incidence of invasive breast cancers should have plummeted with rising detection rates. That has not happened, even though in the pre-mammography era, before about 1980, the number of women found to have D.C.I.S. was only in the hundreds. Nearly 240,000 women receive diagnoses of invasive breast cancer each year.
Those facts lead Dr. Narod to a blunt view. After a surgeon has removed the aberrant cells for the biopsy, he said, “I think the best way to treat D.C.I.S. is to do nothing." ... Others drew back from that advice.
From Medscape: The Mystery of a Common Breast Cancer Statistic
A commonly cited breast cancer statistic — that 30% of all early-stage breast cancers will progress, despite treatment, to deadly metastatic disease — appears to have no strong contemporary evidence to back it up. Nonetheless, the statistic appears widely...."It is estimated that 20% to 30% of all breast cancer cases will become metastatic," said the MBCN in response, repeating a statistic from its own website.
The primary source for this declaration is a 2005 CME review on metastatic disease published in the Oncologist by prominent medical oncologist Joyce O'Shaughnessy, MD, from Baylor University in Houston."Despite advances in the treatment of breast cancer, approximately 30% of women initially diagnosed with earlier stages of breast cancer eventually develop recurrent advanced or metastatic disease," Dr O'Shaughnessy wrote.
According to the National Cancer Institute (NCI), the definition of early-stage breast cancer is that which has not spread beyond the breast or the axillary lymph nodes. The range includes stage I, stage IIA, stage IIB, and stage IIIA disease....According to experts, early breast cancers are known to metastasize at 20 years or beyond.
Dr Brawley worked with two ACS epidemiologists to examine the issue. They looked at breast-cancer-specific mortality (as identified on death certificates) in 12 health districts in the United States from 2008 to 2012. They were surprised by the finding: "28% of the women who died of breast cancer during that time period had localized disease at diagnosis," said Dr Brawley. The result was unexpected. "We all thought 30% was too high," said Dr Brawley.
(NOTE: Photo credit: Wikipedia Commons of Edouard Manet- Blond Woman With Bare Breasts.)

 Of course further studies are needed in humans. But... it is important to note that extra virgin olive oil is viewed as anti-inflammatory and linked to a lower incidence of some cancers, including breast cancer.
Of course further studies are needed in humans. But... it is important to note that extra virgin olive oil is viewed as anti-inflammatory and linked to a lower incidence of some cancers, including breast cancer.
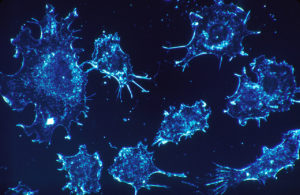 For years medicine has viewed cancer as a "malignant seed" and looked for ways to kill these seeds before they spread throughout the body (metastasis). This past week two provocative articles stresses that we should also look at the "environments" that the cancer cells grow in - that some environments in the person nourish and encourage the growth of cancer, while other environments suppress the growth of cancer and don't allow its spread.
For years medicine has viewed cancer as a "malignant seed" and looked for ways to kill these seeds before they spread throughout the body (metastasis). This past week two provocative articles stresses that we should also look at the "environments" that the cancer cells grow in - that some environments in the person nourish and encourage the growth of cancer, while other environments suppress the growth of cancer and don't allow its spread. For years medicine has viewed cancer as a "
For years medicine has viewed cancer as a " Two recent studies link low vitamin D levels with more aggressive cancers: aggressive prostate cancer in men and more aggressive breast cancers (in mice and women). Researchers generally advise people to take 1000 to 2000 international units per day of vitamin D3 to maintain normal blood levels of of more than 30 nanograms/milliliter. The best source of vitamin D is sunlight, which is why vitamin D is frequently called the sunshine vitamin.
Two recent studies link low vitamin D levels with more aggressive cancers: aggressive prostate cancer in men and more aggressive breast cancers (in mice and women). Researchers generally advise people to take 1000 to 2000 international units per day of vitamin D3 to maintain normal blood levels of of more than 30 nanograms/milliliter. The best source of vitamin D is sunlight, which is why vitamin D is frequently called the sunshine vitamin. A report by 3 prominent specialists (including Gilbert Welch - who has been discussed in earlier
A report by 3 prominent specialists (including Gilbert Welch - who has been discussed in earlier  The issue of overdiagnosis and overtreatment has recently been in the news, especially when discussing breast cancer, prostate cancer, and thyroid cancer. Meaning too much unnecessary treatment with harms, when the best approach would have been to do nothing, as studies have suggested or actually shown. Now here is an article in Medscape suggesting that rather than be quick to operate or treat, the best approach for nearly 70% of prostate cancers may be just "watching".
The issue of overdiagnosis and overtreatment has recently been in the news, especially when discussing breast cancer, prostate cancer, and thyroid cancer. Meaning too much unnecessary treatment with harms, when the best approach would have been to do nothing, as studies have suggested or actually shown. Now here is an article in Medscape suggesting that rather than be quick to operate or treat, the best approach for nearly 70% of prostate cancers may be just "watching". In the past few months there has been a lot of discussion about early screening tests for cancer (when there are no symptoms) versus diagnostic tests (testing once symptoms appear), especially for prostate cancer and breast cancer. Because unfortunately screening also has harms - it is not without significant risks. So the following 2 articles discussing breast cancer are real eye openers. The first article discusses a large study that found that no matter how early the screening and no matter how tiny the cancer and extensive the treatment (e.g, mastectomy of both breasts), in a certain percentage of women the cancer will reappear in a deadly fashion and eventually kill about 3.3% even though they are treated early. The Medscape article points out that it is thought that 28% of early stage breast cancers will progress or reappear as deadly metastatic cancer (even years later) no matter the treatment.
In the past few months there has been a lot of discussion about early screening tests for cancer (when there are no symptoms) versus diagnostic tests (testing once symptoms appear), especially for prostate cancer and breast cancer. Because unfortunately screening also has harms - it is not without significant risks. So the following 2 articles discussing breast cancer are real eye openers. The first article discusses a large study that found that no matter how early the screening and no matter how tiny the cancer and extensive the treatment (e.g, mastectomy of both breasts), in a certain percentage of women the cancer will reappear in a deadly fashion and eventually kill about 3.3% even though they are treated early. The Medscape article points out that it is thought that 28% of early stage breast cancers will progress or reappear as deadly metastatic cancer (even years later) no matter the treatment.