 This study reinforces (once again) that actively playing with toy blocks is good for developing the spatial skills and spatial abilities of children. Other studies have shown that playing with puzzles and actively going out and exploring their environment (like riding a bicycle around the neighborhood) are also good for developing spatial skills and spatial abilities. For both boys and girls. Even though unfortunately this study only looked at 8 year old boys. (Hey, where were the girls???) Remember that playing is how children learn, and helping develop spatial skills is good for math, science, and technology. So get out the Legos and toy blocks and encourage children to play and build! From Medical Xpress:
This study reinforces (once again) that actively playing with toy blocks is good for developing the spatial skills and spatial abilities of children. Other studies have shown that playing with puzzles and actively going out and exploring their environment (like riding a bicycle around the neighborhood) are also good for developing spatial skills and spatial abilities. For both boys and girls. Even though unfortunately this study only looked at 8 year old boys. (Hey, where were the girls???) Remember that playing is how children learn, and helping develop spatial skills is good for math, science, and technology. So get out the Legos and toy blocks and encourage children to play and build! From Medical Xpress:
Neuroimaging study: Building blocks activate spatial ability in children better than board games
Research from Indiana University has found that structured block-building games improve spatial abilities in children to a greater degree than board games. The study, which appears in the journal Frontiers in Psychology, measured the relative impact of two games—a structured block-building game and a word-spelling board game—on children's spatial processing, including mental rotation, which involves visualizing what an object will look like after it is rotated. The research lends new support to the idea that such block games might help children develop spatial skills needed in science- and math-oriented disciplines.
Block play changed brain activation patterns," Newman said. "It changed the way the children were solving the mental rotation problems; we saw increased activation in regions that have been linked to spatial processing only in the building blocks group." The structured block-building game used for the study was called "Blocks Rock"; the board game was Scrabble.
The research builds upon previous studies that have shown that children who frequently participate in activities such as block play, puzzles and board games have higher spatial ability than those who participate more in activities such as drawing, riding bikes, or playing with trucks and sound-producing toys.
It is also demonstrates that training on one visuo-spatial task can transfer to other tasks. In this instance, training on the structured block-building game resulted in transfer to mental rotation performance.....To conduct the study, IU researchers placed 28 8-year-olds in a magnetic resonance imaging scanner before and after playing one of the two games. Play sessions were conducted for 30 minutes over the course of five days.
There were no differences in mental rotation performance between the two groups in either the brain activation or performance during the first rotation test and scan. But the block play group showed a change in activation in regions linked to both motor and spatial processing during the second scan. The group who played board games failed to show any significant change in brain activation between the pre- and post-game scans, or any significant improvement on the mental rotation test results.
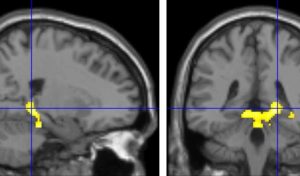 Scans of the children's brains show increased activation in the anterior lobe of the cerebellum and the parahippocampus during the second mental rotation test, which was administered after they played with blocks. Credit: Indiana University
Scans of the children's brains show increased activation in the anterior lobe of the cerebellum and the parahippocampus during the second mental rotation test, which was administered after they played with blocks. Credit: Indiana University

 The big scary question: What will happen after antibiotics cease to work? And people start dying by the millions from infections that used to be easily treated? We are fast approaching that point of total antibiotic resistance, with superbugs that resist all antibiotics. More and more disease-causing bacteria are rapidly evolving immunity to every existing antibiotic (see
The big scary question: What will happen after antibiotics cease to work? And people start dying by the millions from infections that used to be easily treated? We are fast approaching that point of total antibiotic resistance, with superbugs that resist all antibiotics. More and more disease-causing bacteria are rapidly evolving immunity to every existing antibiotic (see  Ten chemicals suspected or known to harm human health are present in more than 90% of U.S. household dust samples, according to a new study. The research adds to a growing body of evidence showing the dangers posed by exposure to chemicals we are exposed to on a daily basis. The chemicals come from a variety of household goods, including toys, cosmetics, personal care products, furniture, electronics, nonstick cookware, food packaging, floor coverings, some clothing (e.g., stain resistant), building materials, and cleaning products. How do the chemicals get into the dust? The chemicals can leach, migrate, abrade, or off-gas from the products, which winds up in the dust and results in human exposure. (That's right: vacuum a lot and wash your hands a lot, and try to avoid or cut back use of products with these chemicals,)
Ten chemicals suspected or known to harm human health are present in more than 90% of U.S. household dust samples, according to a new study. The research adds to a growing body of evidence showing the dangers posed by exposure to chemicals we are exposed to on a daily basis. The chemicals come from a variety of household goods, including toys, cosmetics, personal care products, furniture, electronics, nonstick cookware, food packaging, floor coverings, some clothing (e.g., stain resistant), building materials, and cleaning products. How do the chemicals get into the dust? The chemicals can leach, migrate, abrade, or off-gas from the products, which winds up in the dust and results in human exposure. (That's right: vacuum a lot and wash your hands a lot, and try to avoid or cut back use of products with these chemicals,) This is similar to what Dr. Gilbert Welch and others have been saying for a while - that studies show much cancer screening leads to overdiagnosis and overtreatment with no real differences in rates of mortality (death). Which was the whole point of cancer screening - to catch cancers early and so reduce rates of death. (For more on this topic see
This is similar to what Dr. Gilbert Welch and others have been saying for a while - that studies show much cancer screening leads to overdiagnosis and overtreatment with no real differences in rates of mortality (death). Which was the whole point of cancer screening - to catch cancers early and so reduce rates of death. (For more on this topic see .jpg) There are some things we can do that are linked to living longer, such as not smoking and exercising regularly, but could reading books also have such an effect?
There are some things we can do that are linked to living longer, such as not smoking and exercising regularly, but could reading books also have such an effect?  It has long been known that laser pointers can be damaging to the eyes, but apparently this is not widely known. Injuries to the eyes (retinal injuries) causing irreversible vision loss are rapidly increasing from them, especially among children. Injuries to the eye happen when a person stares directly into the laser pointer, or even into the reflection in a mirror. This can inadvertently happen among children, for example when playing games such as laser tag.
It has long been known that laser pointers can be damaging to the eyes, but apparently this is not widely known. Injuries to the eyes (retinal injuries) causing irreversible vision loss are rapidly increasing from them, especially among children. Injuries to the eye happen when a person stares directly into the laser pointer, or even into the reflection in a mirror. This can inadvertently happen among children, for example when playing games such as laser tag. The latest development in treating stubborn cases of Clostridium difficile infections (CDI) are "poop pills" - pills that patients can easily swallow rather than having to go through a fecal microbiota transplant (FMT). The "poop pills" are filled with blenderized fecal matter from healthy donors, are much easier for patients to swallow, and they successfully treat C. difficile at almost the same rate as fecal microbiota transplants - about 91% after 1 or 2 treatments for the pills, and 93 to 96% for FMT. This is an amazing success rate for an infection that debilitates people, is resistant to antibiotics in many cases, and even kills people.
The latest development in treating stubborn cases of Clostridium difficile infections (CDI) are "poop pills" - pills that patients can easily swallow rather than having to go through a fecal microbiota transplant (FMT). The "poop pills" are filled with blenderized fecal matter from healthy donors, are much easier for patients to swallow, and they successfully treat C. difficile at almost the same rate as fecal microbiota transplants - about 91% after 1 or 2 treatments for the pills, and 93 to 96% for FMT. This is an amazing success rate for an infection that debilitates people, is resistant to antibiotics in many cases, and even kills people. Here is an amazing short video for those interested in seeing how bacteria mutate and grow when exposed to antibiotics - and evolving to become superbugs. Researchers filmed an experiment that created bacteria a thousand times more drug-resistant than their ancestors. In the time-lapse video, a white bacterial colony (E.coli bacteria) creeps across an enormous black petri dish plated with vertical bands of successively higher doses of antibacterial drugs (antibiotics).
Here is an amazing short video for those interested in seeing how bacteria mutate and grow when exposed to antibiotics - and evolving to become superbugs. Researchers filmed an experiment that created bacteria a thousand times more drug-resistant than their ancestors. In the time-lapse video, a white bacterial colony (E.coli bacteria) creeps across an enormous black petri dish plated with vertical bands of successively higher doses of antibacterial drugs (antibiotics). Over the years I have read about some oils, especially lavender and tea tree oils, as having hormone altering (endocrine disrupting) effects when used over prolonged periods of time or when someone is "chronically exposed". Especially worrisome was the possible estrogenic effects of lavender oils in shampoos, lotions, and soaps on developing children - especially boys (prolonged use leading to the development of breasts in some boys!). I just read a recently published journal study (with very interesting comments at the end), and an article in WebMD about this same topic. The condition of early breast development is called prepubertal gynecomastia in boys and thelarche in girls.
Over the years I have read about some oils, especially lavender and tea tree oils, as having hormone altering (endocrine disrupting) effects when used over prolonged periods of time or when someone is "chronically exposed". Especially worrisome was the possible estrogenic effects of lavender oils in shampoos, lotions, and soaps on developing children - especially boys (prolonged use leading to the development of breasts in some boys!). I just read a recently published journal study (with very interesting comments at the end), and an article in WebMD about this same topic. The condition of early breast development is called prepubertal gynecomastia in boys and thelarche in girls. This article by Dr. Thomas E. Finucane lays out nicely a paradigm shift in how to view uncomplicated urinary tract infections (UTIs) - as a case of dysbiosis (microbial community out of whack), and that antibiotics to kill bacteria are generally not needed or helpful. (He doesn't mention it, but the next step in his argument should be that probiotic or beneficial bacteria or other microbes may improve the microbial community and symptoms.) A main point of the article is that we now know the urinary tract is not sterile - instead diverse microbiota live there (the microbial community is the
This article by Dr. Thomas E. Finucane lays out nicely a paradigm shift in how to view uncomplicated urinary tract infections (UTIs) - as a case of dysbiosis (microbial community out of whack), and that antibiotics to kill bacteria are generally not needed or helpful. (He doesn't mention it, but the next step in his argument should be that probiotic or beneficial bacteria or other microbes may improve the microbial community and symptoms.) A main point of the article is that we now know the urinary tract is not sterile - instead diverse microbiota live there (the microbial community is the