 Human brains are getting larger each decade. That's the conclusion of researchers conducting the large Framingham Heart study which has now gone on for 75 years.
Human brains are getting larger each decade. That's the conclusion of researchers conducting the large Framingham Heart study which has now gone on for 75 years.
Between 1999 and 2019 the researchers conducted MRIs on participants born from the 1930s to the 1970s, with participants having an average age of 57. They found that each decade the brain volume steadily increased, with the brains of people born in the 1970s having 6.6% more volume than those born in the 1930s. Brain surface area increased about 15% in that time.
Brain structures such as white matter, gray matter, and hippocampus (a brain region involved in learning and memory) also increased in size over time. This increase in brain volume clearly shows that environmental factors (e.g., nutrition, education, social), and not just genetic factors, influence brain size.
The researchers thought that a larger brain volume, which signifies brain health, might be protective against Alzheimer's disease. And that this could explain why the percentage of people (the incidence) of Alzheimer's disease and dementia has gone down over time.
From Medical Xpress: Human brains are getting larger: That may be good news for dementia risk
A new study by researchers at UC Davis Health found human brains are getting larger. Study participants born in the 1970s had 6.6% larger brain volumes and almost 15% larger brain surface area than those born in the 1930s. ...continue reading "Human Brains Are Getting Larger Over Time"

 Choline appears to be a neglected nutrient. It is essential for healthy brain functioning, yet researchers of a
Choline appears to be a neglected nutrient. It is essential for healthy brain functioning, yet researchers of a  A recent study found that eating higher levels of foods with flavonoids (e.g. berries, apples, and tea) may lower the risk of later development of Alzheimer's disease and other age-related dementias.
A recent study found that eating higher levels of foods with flavonoids (e.g. berries, apples, and tea) may lower the risk of later development of Alzheimer's disease and other age-related dementias.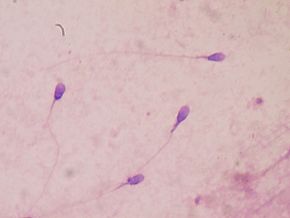 Are we heading toward a time in the not so distant future when all men are infertile? (Due to exposure to all the endocrine disruptors around us.)
Are we heading toward a time in the not so distant future when all men are infertile? (Due to exposure to all the endocrine disruptors around us.)  Type 2 Diabetes May Be Reversed With Weight Loss
Type 2 Diabetes May Be Reversed With Weight Loss More and more evidence is accumulating that certain diets are anti-inflammatory. Especially beneficial are diets rich in fruits, vegetables, seeds, nuts, legumes (beans), and whole grains - which also have a lot of fiber. This is exciting research because chronic low-grade inflammation is linked to a number of chronic diseases (heart disease, cancer, etc.).
More and more evidence is accumulating that certain diets are anti-inflammatory. Especially beneficial are diets rich in fruits, vegetables, seeds, nuts, legumes (beans), and whole grains - which also have a lot of fiber. This is exciting research because chronic low-grade inflammation is linked to a number of chronic diseases (heart disease, cancer, etc.).