 We all know that exercise is beneficial for health. Research suggests that exercising out in nature is best for several varied reasons - including that it lowers markers of inflammation, and that it's good for our gut microbiome (community of gut microbes). The following excerpts are written by Dr. John La Puma encouraging other doctors to prescribe exercise for their patients and why.
We all know that exercise is beneficial for health. Research suggests that exercising out in nature is best for several varied reasons - including that it lowers markers of inflammation, and that it's good for our gut microbiome (community of gut microbes). The following excerpts are written by Dr. John La Puma encouraging other doctors to prescribe exercise for their patients and why.
An important message of his is that exercise is more important than a drug prescription for a number of conditions, including diabetes prevention, reducing the risk of recurrence of several cancers (he mentions breast cancer, but it also holds for prostate cancer). While exercising and walking out in nature may be best, any exercise anywhere is better than no exercise. (Other posts on exercise as prescription medicine are here and here; and check the category exercise for all exercise research posts).
From Medscape: Rx: Exercise Daily -- Outdoors. Doctor's Orders
With dazzling Olympic feats on display all summer, too many of my patients are still literally immobilized. Medically, sitting too long shuts off the enzyme lipoprotein lipase. In people who are sedentary, the enzyme doesn't break down fat to create energy, like it should. But medical prescription for exercise has lagged even the slowest runner. Why? Some reasons are time, training, and money. Time especially is a scarce commodity: The average clinician visit lasts just 20 minutes. Fitness is a shamefully small part of medical training. And as doctors, we don't get paid for discussing exercise, let alone monitoring a prescription and assessing the response.
Finally, there are practical reasons. Clinicians find it difficult to persuade patients that exercise is more effective than medication for any number of conditions, including stroke recovery, diabetes prevention, and treatment of low back pain. Regular exercise reduces the risk for recurrent breast cancer by approximately 50%. Given all these reasons, it's easy to see why fitness prescriptions are seldom more than an afterthought. Yet even without formally prescribing the frequency, intensity, time, and type of exercise, clinicians can speak with patients and families about fitness in inspiring, life-changing ways.
Because clinicians have a secret weapon to use that most people don't even know about—location. Exercising in nature (in sight of and preferably near water or greenery, whether a deserted beach or an urban park) is better. Walking city streets and the office itself can be harder on your health than you think. In both environments, your attention is demanded and directed—sometimes by digital interruptions, sometimes by vehicles, toxins, or duties. In nature, your attention is drawn, not pushed, to a variety of often unexpected but not unpleasant sounds, colors, aromas, textures, and forms.
A recent Stanford study of nature therapy showed significantly reduced rumination after a 90-minute walk in nature, compared with a 90-minute walk through an urban environment. On MRI, "nature walkers" showed lower activity in an area of the brain linked to risk for mental illness, the subgenual prefrontal cortex, compared with "urban walkers." In other words, nature offers a sense of something bigger than ourselves on which to focus. MRIs show the way the brain changes when that sense occurs to us.
Exercising in nature may improve a person's immune system by enriching the diversity in the microbiota. Microbiota buffer the immune system against chronic stress-related disease. They appear to act as a hormone-producing organ, not simply a collection of beneficial bacteria. Microbiota are sensitive and responsive to physical environmental changes as well as dietary ones. So, exercise in nature may favorably boost microbiota.
And finally, exercise in nature is clinically preferred and calming. A Norwegian study showed that exercise in nature and in view of nature improves both mood and diastolic blood pressure vs exercise without nature. A Chinese study showed higher energy levels, and lower levels of interleukin-6 and tumor necrosis factor (both markers of inflammation), in a forest walking group compared with an urban exercising group. A British study showed significantly improved mood and self-esteem with "green" exercise, with the largest benefits from 5-minute engagements. Five minutes!
Of course, there are areas in our country and world in which it is dangerous to walk, never mind exercise. It may not be as easy to generate sweat and intensity with outdoor exercise as it is with indoor exercise. It may be stormy, or baking hot, or otherwise harsh outside, and the cool recesses of one's own bedroom or the gym may be just perfect for you today. And with the 2013 total cost of inactivity estimated at $24.7 billion for the United States, and with the public sector bearing almost one half of that expense, any exercise anywhere is better than none. Yet physicians have a therapeutic tool few others in our culture wield—a prescription pad—and we have every patient's attention, at least for a few minutes. Patients try harder when doctors advise them about fitness.

 Ten chemicals suspected or known to harm human health are present in more than 90% of U.S. household dust samples, according to a new study. The research adds to a growing body of evidence showing the dangers posed by exposure to chemicals we are exposed to on a daily basis. The chemicals come from a variety of household goods, including toys, cosmetics, personal care products, furniture, electronics, nonstick cookware, food packaging, floor coverings, some clothing (e.g., stain resistant), building materials, and cleaning products. How do the chemicals get into the dust? The chemicals can leach, migrate, abrade, or off-gas from the products, which winds up in the dust and results in human exposure. (That's right: vacuum a lot and wash your hands a lot, and try to avoid or cut back use of products with these chemicals,)
Ten chemicals suspected or known to harm human health are present in more than 90% of U.S. household dust samples, according to a new study. The research adds to a growing body of evidence showing the dangers posed by exposure to chemicals we are exposed to on a daily basis. The chemicals come from a variety of household goods, including toys, cosmetics, personal care products, furniture, electronics, nonstick cookware, food packaging, floor coverings, some clothing (e.g., stain resistant), building materials, and cleaning products. How do the chemicals get into the dust? The chemicals can leach, migrate, abrade, or off-gas from the products, which winds up in the dust and results in human exposure. (That's right: vacuum a lot and wash your hands a lot, and try to avoid or cut back use of products with these chemicals,) This is similar to what Dr. Gilbert Welch and others have been saying for a while - that studies show much cancer screening leads to overdiagnosis and overtreatment with no real differences in rates of mortality (death). Which was the whole point of cancer screening - to catch cancers early and so reduce rates of death. (For more on this topic see
This is similar to what Dr. Gilbert Welch and others have been saying for a while - that studies show much cancer screening leads to overdiagnosis and overtreatment with no real differences in rates of mortality (death). Which was the whole point of cancer screening - to catch cancers early and so reduce rates of death. (For more on this topic see  Yikes! A good reason to lose weight now rather than years from now, and the importance of not ignoring a weight gain (you know, over the years as the pounds slowly creep up). The researchers found that for every 10 years of being overweight as an adult, there was an associated 7% increase in the risk for all obesity-related cancers. The degree of overweight (dose-response) during adulthood was important in the risk of developing cancer, especially for
Yikes! A good reason to lose weight now rather than years from now, and the importance of not ignoring a weight gain (you know, over the years as the pounds slowly creep up). The researchers found that for every 10 years of being overweight as an adult, there was an associated 7% increase in the risk for all obesity-related cancers. The degree of overweight (dose-response) during adulthood was important in the risk of developing cancer, especially for 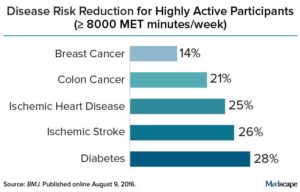 Credit: Medscape
Credit: Medscape Yup, according to a new mega-study, being overweight or obese is linked to higher risk of dying prematurely than being normal weight. And the more you weigh, the greater the risk.
Yup, according to a new mega-study, being overweight or obese is linked to higher risk of dying prematurely than being normal weight. And the more you weigh, the greater the risk.