 Something new to add to the list of what is in our skin microbiome - the community of microbes (bacteria, fungi, viruses) living on our skin. It turns out we also have archaea, which are single-celled microorganisms that are thought to be beneficial. (Earlier post on archaea found in our bodies.)
Something new to add to the list of what is in our skin microbiome - the community of microbes (bacteria, fungi, viruses) living on our skin. It turns out we also have archaea, which are single-celled microorganisms that are thought to be beneficial. (Earlier post on archaea found in our bodies.)
The human skin microbiome acts as a barrier protecting our body from pathogens and other environmental influences. The most common archaea found in the samples (from the chest area of 51 volunteers between the ages of 1 to 75 years) is called Thaumarchaeota. The results reveal that archaea are more abundant in people older than 60 years or younger than 12 years (as compared to middle-aged persons). But there were no differences between males and females. From Science Daily:
What's on your skin? Archaea, that's what
It turns out your skin is crawling with single-celled microorganisms -- and they're not just bacteria. A study by the Department of Energy's Lawrence Berkeley National Laboratory (Berkeley Lab) and the Medical University of Graz has found that the skin microbiome also contains archaea, a type of extreme-loving microbe, and that the amount of it varies with age. The researchers conducted both genetic and chemical analyses of samples collected from human volunteers ranging in age from 1 to 75. They found that archaea (pronounced ar-KEY-uh) were most abundant in subjects younger than 12 and older than 60.
In addition to the influence of age, they found that gender was not a factor but that people with dry skin have more archaea. "Archaea might be important for the cleanup process under dry skin conditions," said Moissl-Eichinger. "The results of our genetic analysis (DNA-based quantitative PCR and next-generation sequencing), together with results obtained from infrared spectroscopy imaging, allowed us to link lower levels of sebum [the oily secretion of sebaceous glands] and thus reduced skin moisture with an increase of archaeal signatures."
It was not until the 1970s that scientists realized how different archaea were from bacteria, and they became a separate branch on the tree of life -- the three branches being Bacteria, Archaea, and Eukarya (which includes all plants and animals). Archaea are commonly found in extreme environments, such as hot springs and Antarctic ice. Nowadays it is known that archaea exist in sediments and in Earth's subsurface as well, but they have only recently been found in the human gut and linked with the human microbiome.
Their study focused on Thaumarchaeota, one of the many phyla of archaea, as little evidence of the others was found in the pilot study. "We know that Thaumarchaeota are supposed to be an ammonia-oxidizing microorganism, and ammonia is a major component of sweat, which means they might play a role in nitrogen turnover and skin health," Holman said. .... the team also correlated archaeal abundance with skin dryness, as middle-aged persons have higher sebum levels and thus moister skin than the elderly. So far, most archaea are known to be beneficial rather than harmful to human health. They may be important for reducing skin pH or keeping it at low levels, and lower pH is associated with lower susceptibility to infections. [Original study.]
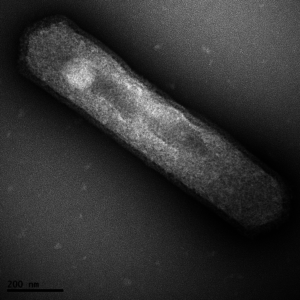
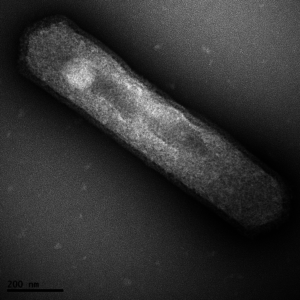 Thaumarchaeota archaea. These single-celled organisms have just one membrane sac that encloses their bodies. Credit: Univ. of Washington
Thaumarchaeota archaea. These single-celled organisms have just one membrane sac that encloses their bodies. Credit: Univ. of Washington

 The following article is about Dr. Janelle Ayres, a researcher in California, working on "beneficial bacteria" to help the body tolerate infections. This is different than the usual medical approach of fighting infections - where antibiotics are used to kill microbes. Reading the article, my first thought was "Well, duh....of course this approach works." This is what we've been doing in using
The following article is about Dr. Janelle Ayres, a researcher in California, working on "beneficial bacteria" to help the body tolerate infections. This is different than the usual medical approach of fighting infections - where antibiotics are used to kill microbes. Reading the article, my first thought was "Well, duh....of course this approach works." This is what we've been doing in using  Hah! A study that builds on what is already known by many women - that the non-prescription product D-mannose works for urinary tract infections (UTIs). D-mannose is amazingly effective for urinary tract infections caused by E. coli bacteria (up to 90% of UTIs), even infections that keep recurring (30 to 50% of infections), and which don't respond to numerous antibiotics.
Hah! A study that builds on what is already known by many women - that the non-prescription product D-mannose works for urinary tract infections (UTIs). D-mannose is amazingly effective for urinary tract infections caused by E. coli bacteria (up to 90% of UTIs), even infections that keep recurring (30 to 50% of infections), and which don't respond to numerous antibiotics. Great idea and one that this blog has been pushing for a long time - the use of
Great idea and one that this blog has been pushing for a long time - the use of  Stop using the damn antibacterial products! Yes, stop using stuff that says "antibacterial", "antimicrobial", "germ-killing", or "anti-odor". Whether in personal care items, or bedding, or socks, or hand wipes, or wherever else you see those labels - don't buy them and try to avoid using them. Plain soap works just as well for cleaning hands (see
Stop using the damn antibacterial products! Yes, stop using stuff that says "antibacterial", "antimicrobial", "germ-killing", or "anti-odor". Whether in personal care items, or bedding, or socks, or hand wipes, or wherever else you see those labels - don't buy them and try to avoid using them. Plain soap works just as well for cleaning hands (see  OK, the study results sound promising: that washing with cold water is as good as washing with warm or hot water for removing bacteria from the hands. And that type of soap didn't matter - both the anti-microbial soap and ordinary soap were equally effective. But...the researchers only looked at one strain of bacteria - E. coli (full name Escherichia coli (ATCC 11229)), and there are MANY microbes and viruses out there that cause problems. So I would view it as a nice start ( a preliminary study), but not the final word. From Science Daily:
OK, the study results sound promising: that washing with cold water is as good as washing with warm or hot water for removing bacteria from the hands. And that type of soap didn't matter - both the anti-microbial soap and ordinary soap were equally effective. But...the researchers only looked at one strain of bacteria - E. coli (full name Escherichia coli (ATCC 11229)), and there are MANY microbes and viruses out there that cause problems. So I would view it as a nice start ( a preliminary study), but not the final word. From Science Daily: An amazing new study is about to start in Sweden - this study will see if "snot transplants" work for the treatment for chronic sinusitis! Will this turn out to be a permanent treatment? While
An amazing new study is about to start in Sweden - this study will see if "snot transplants" work for the treatment for chronic sinusitis! Will this turn out to be a permanent treatment? While 
