 Eating lots of fruits and vegetables (more than 10 servings a day!) is linked to better cognitive functioning in both normal weight and overweight adults (both young and older adults), and may delay the onset of cognitive decline that occurs with aging and also dementia. Overweight and obese older adults with a daily fruit and vegetable consumption of less than 5 servings generally had worse cognitive functioning. Higher levels of physical activity and higher daily fruit and vegetable consumption were both associated with better cognitive functioning. Cognitive functioning generally refers to a person’s ability to reason and think, the mental processes needed to gather and process information, and all aspects of language and memory.
Eating lots of fruits and vegetables (more than 10 servings a day!) is linked to better cognitive functioning in both normal weight and overweight adults (both young and older adults), and may delay the onset of cognitive decline that occurs with aging and also dementia. Overweight and obese older adults with a daily fruit and vegetable consumption of less than 5 servings generally had worse cognitive functioning. Higher levels of physical activity and higher daily fruit and vegetable consumption were both associated with better cognitive functioning. Cognitive functioning generally refers to a person’s ability to reason and think, the mental processes needed to gather and process information, and all aspects of language and memory.
The York University researchers found that fruit and vegetable consumption, physical activity, and BMI or body mass index (normal, overweight, obese) all appear to interact in how a person mentally functions (cognitive functioning), especially as they age. The ideal goal as one ages is to preserve the mind. It appears that eating lots of fruits and vegetables daily (10 or more servings), being physically active (this includes daily walks), and being a healthy weight help with this goal. It helps to also be highly educated (or read books?) so that the brain has a "cognitive reserve",
Why is daily fruit and vegetable consumption (FVC) good for cognitive functioning and the brain? Studies find that daily consumption of fruits and vegetables is strongly associated with a reduced risk of cardiovascular disease, cancer, diabetes and age-related declines. They appear to be "protective" against cognitive decline. The study researchers point out that fruits and vegetables contain high quantities of vitamin C and E, fiber, micronutrients, flavonoids, beta-carotenes and other classes of phytochemicals. These are important in various ways: "they modulate detoxifying enzymes, stimulate the immune system, modulate cholesterol synthesis, and act as antibacterial, antioxidant or neuroprotective agents." NOTE: A serving of fruit is generally 1 medium fruit or 1/2 cup of fruit. A serving of vegetables is 1 cup of raw leafy greens or 1/2 cup of other vegetables. From Medical Xpress:
Healthy living linked to higher brain function, delay of dementia
It's tempting to dip into the leftover Halloween treats, but new research out of York University has found eating plenty of fruits and vegetables, combined with regular exercise, leads to better cognitive functioning for younger and older adults, and may delay the onset of dementia. York U post-doctoral fellow Alina Cohen and her team, including Professors Chris I. Ardern and Joseph Baker, looked at cross-sectional data of 45,522 participants, age 30 to 80+, from the 2012 annual component of the Canadian Community Health Survey.
What they found was that for those who are normal weight or overweight, but not obese, eating more than 10 servings of fruit and vegetable daily was linked to better cognitive functioning. When moderate exercise was added, those eating less than five servings, reported better cognitive functioning. Higher levels of physical activity were linked to the relationship between higher daily fruit and vegetable consumption and better cognitive performance. Those with higher body mass indexes, low activity levels and fruit and vegetable consumption were associated with poorer cognitive functioning.
More details from the original study in the Journal of Public Health: Physical activity mediates the relationship between fruit and vegetable consumption and cognitive functioning: a cross-sectional analysis
Results: Higher BMIs, lower PA [physical activity] and FVC [fruit and vegetable consumption] were associated with poorer cognitive functioning. Additionally, PA statistically mediated the relationship between FVC and cognitive function (Sobel test: t = −3.15; P < 0.002); and higher education levels and daily FVC were associated with better cognitive function (P < 0.001). Conclusion: Higher PA levels were associated with better cognitive functioning in younger and older adults. Also, higher daily FVC and education levels were associated with better cognitive scores.
Individuals who were normal weight or overweight and reported a FVC of >10 servings per day reported better cognitive functioning scores than those who reported <10 servings, as well as those individuals with obesity . As well, both active and inactive individuals who reported a FVC of >10 servings per day had better cognitive scores than those who consumed fewer servings. However, in those who were moderately active, individuals with a daily FVC of <5 or 5–10 servings reported better cognitive functioning than those with a daily FVC of 10 or more servings; this may have resulted because of underestimations of the number of servings of fruits and vegetables actually consumed... Thus, increasing FVC and PA levels as well as having a healthy BMI may aid in the delay of cognitive decline.
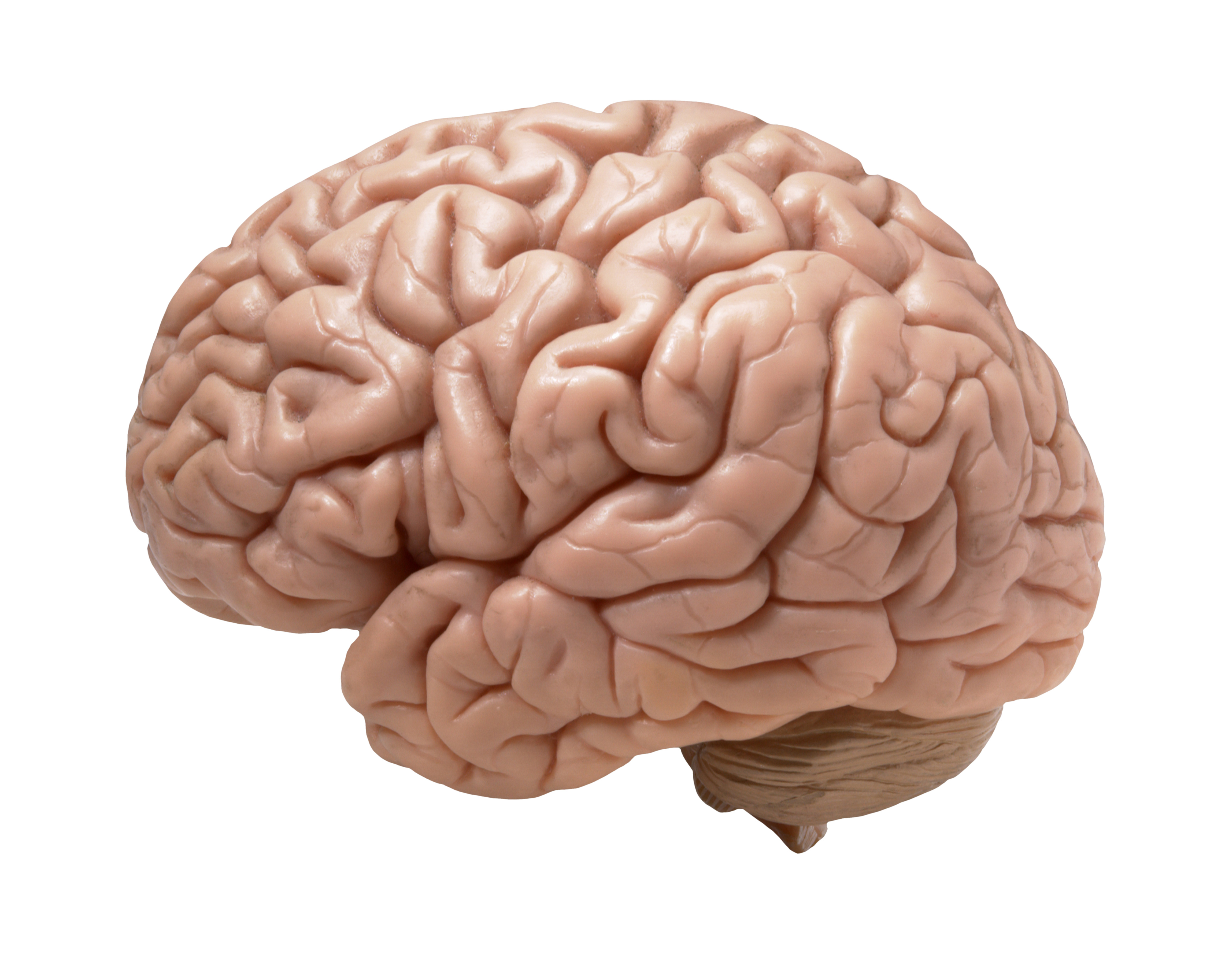
Results also indicated that higher education levels along with a daily FVC of five or more servings were associated with better cognitive functioning. Education may be assisting in the process of delaying cognitive decline by increasing cognitive reserve, the ability of the human brain to cope with damage by using different brain processes to retain the ability to function well. Cognitive reserve is developed through intellectual stimulation and translates into a higher volume of connections between neurons and stronger rates of cerebral blood flow.
 An interesting study looked at what the act of walking does to our brain, and found that it can modify and increase the amount of blood that’s sent to the brain (which is viewed as beneficial for brain function). The study, performed by researchers at New Mexico Highlands University in the United States, found that the foot’s impact on the ground while walking sends pressure waves through the arteries, which can increase the blood supply to the brain. This is referred to as cerebral blood flow or CBF.
An interesting study looked at what the act of walking does to our brain, and found that it can modify and increase the amount of blood that’s sent to the brain (which is viewed as beneficial for brain function). The study, performed by researchers at New Mexico Highlands University in the United States, found that the foot’s impact on the ground while walking sends pressure waves through the arteries, which can increase the blood supply to the brain. This is referred to as cerebral blood flow or CBF.
 Once again, research supports that you should get off your butt and exercise! Or do a moderate to vigorous physical activity at least several times a week, which can include housework, gardening, dancing, swimming, or walking briskly. Most important is to MOVE. And why is this so important? Not just for physical health and prevention of certain diseases, but also for the health of your brain, especially as it ages.
Once again, research supports that you should get off your butt and exercise! Or do a moderate to vigorous physical activity at least several times a week, which can include housework, gardening, dancing, swimming, or walking briskly. Most important is to MOVE. And why is this so important? Not just for physical health and prevention of certain diseases, but also for the health of your brain, especially as it ages. Heart attacks run in the family? Does this mean you are doomed to also have a heart attack? Well, the good news from a large study is that a healthy lifestyle (with at least 3 of these 4 behaviors: not currently smoking, not being obese, regular physical activity at least once per week, and eating a good diet) lowers the risk of a heart attack by nearly 50% even in those with a high genetic risk for heart attacks. (This is compared to those with an unhealthy lifestyle, which is none or only one healthy behavior.) In this study a
Heart attacks run in the family? Does this mean you are doomed to also have a heart attack? Well, the good news from a large study is that a healthy lifestyle (with at least 3 of these 4 behaviors: not currently smoking, not being obese, regular physical activity at least once per week, and eating a good diet) lowers the risk of a heart attack by nearly 50% even in those with a high genetic risk for heart attacks. (This is compared to those with an unhealthy lifestyle, which is none or only one healthy behavior.) In this study a  Eating lots of fruits and vegetables (more than 10 servings a day!) is linked to better cognitive functioning in both normal weight and overweight adults (both young and older adults), and may delay the onset of cognitive decline that occurs with aging and also dementia.
Eating lots of fruits and vegetables (more than 10 servings a day!) is linked to better cognitive functioning in both normal weight and overweight adults (both young and older adults), and may delay the onset of cognitive decline that occurs with aging and also dementia.  Another study finding brain changes from playing tackle football - this time measurable brain changes were found in boys 8 to 13 years old after just one season of playing football. None of the boys had received a concussion diagnosis during the season. The changes in the white matter of the brain (and detected with magnetic resonance imaging (MRI) were from the cumulative subconcussive head impacts that occur in football - the result of repetitive hits to the head during games and practices.
Another study finding brain changes from playing tackle football - this time measurable brain changes were found in boys 8 to 13 years old after just one season of playing football. None of the boys had received a concussion diagnosis during the season. The changes in the white matter of the brain (and detected with magnetic resonance imaging (MRI) were from the cumulative subconcussive head impacts that occur in football - the result of repetitive hits to the head during games and practices.