 A thought-provoking article by Heiman and Greenway was just published in the journal Molecular Metabolism making the case that changes in farming practices over the last 50 years have resulted in decreased agricultural diversity which, in turn, has resulted in decreased dietary diversity, and that the reduction in dietary diversity has changed and decreased the richness of the human gut microbiota (microbes living in the gut). And meanwhile, during the past 50 years, the rates of obesity, type 2 diabetes, and inflammatory bowel diseases sharply increased - and in each of these conditions there is a reduction of the gut microbial diversity. Similar views have also been stated by others in the field of microbiology.
A thought-provoking article by Heiman and Greenway was just published in the journal Molecular Metabolism making the case that changes in farming practices over the last 50 years have resulted in decreased agricultural diversity which, in turn, has resulted in decreased dietary diversity, and that the reduction in dietary diversity has changed and decreased the richness of the human gut microbiota (microbes living in the gut). And meanwhile, during the past 50 years, the rates of obesity, type 2 diabetes, and inflammatory bowel diseases sharply increased - and in each of these conditions there is a reduction of the gut microbial diversity. Similar views have also been stated by others in the field of microbiology.
The thinking is that the more diverse the diet, the more diverse the gut microbiome (and healthier), and the more it can adapt to disturbances. Heiman and Greenway state: "Unfortunately, dietary diversity has been lost during the past 50 years because of economic pressures for greater food production to support a growing world population.... Of the 250,000 to 300,000 known edible plant species, humans use only 150 to 200...Today, 75 percent of the world's food is generated from only 12 plants and five animal species."
Also, agricultural practices of using antibiotics as growth promoters for poultry, swine, and cattle further harm the human gut microbiome when the meat is ingested by humans, and pesticide residues on crops ingested by humans may have gut microbiome effects. Even emulsifiers, used in processed foods, reduce microbial richness. Every time a person goes on a certain diet (vegan, Paleo, etc) or makes dietary choices in which some foods are eliminated, it makes it easier for some microbial species, and gives them a competitive advantage over other gut microbes. From Science Daily:
Reduction in dietary diversity impacts richness of human gut microbiota
Changes in farming practices over the last 50 years have resulted in decreased agro-diversity which, in turn, has resulted in decreased dietary diversity. The significant impact of this change in dietary richness on human health is an emerging topic for discussion
Heiman and Greenway describe how the reduction in dietary diversity has changed the richness of human gut microbiota, the community of microorganisms living in the gut. The researchers point out that healthy individuals have diverse gut microbiota and many of the common pathologies of the 21st century, including type 2 diabetes, obesity and inflammatory bowel disease, are associated with reduced microbiotic richness.
Gut microbiota function as an endocrine organ, metabolizing specific nutrients from the diet and producing specific substances that act as metabolic signals in the host. It follows then that highly specialized diets will change the landscape of the gut microbiome over time. In fact, it takes only a few days of changing diet to alter the microbiotic makeup of the human gut. And if the dietary change involves elimination of one or more macronutrients (think Atkins or Paleo or vegan), humans are essentially selecting for some microbiotic species over others.
The importance of microbiota diversity cannot be overstated. They produce an abundance of important molecules for the host and with increased variation comes increased adaptability and an increased range of physiological responses. "The greater the repertoire of signals, the more likely is the ability to maintain homeostasis when dietary intake is perturbed," explain Heiman and Greenway. "Furthermore, because each particular macronutrient has the potential to be metabolized by microbiota into unique metabolic signals, the greater the variety in signals, the greater the variety of responses possible."

 Two articles about the link between Alzheimer's disease (AD) and microbes this past week: a study linking periodontal disease and Alzheimer's, and the other a journal editorial (written by an international team of 31 researchers) suggesting that we need to more closely look at the role of microbes in Alzheimer's disease, especially herpes virus, chlamydia and spirochaete bacteria.
Two articles about the link between Alzheimer's disease (AD) and microbes this past week: a study linking periodontal disease and Alzheimer's, and the other a journal editorial (written by an international team of 31 researchers) suggesting that we need to more closely look at the role of microbes in Alzheimer's disease, especially herpes virus, chlamydia and spirochaete bacteria. Very exciting research IF it pans out - the idea of treating (some) cancers with probiotics (beneficial bacteria). This study was done on mice, and some mice started the probiotic mixture one week before they gave the mice the liver cancer, so...more limitations there. But the idea is so tantalizing and wonderful... And what was in the mixture of bacteria (called probiotic Prohep) that the mice ate that had beneficial results of shrinking liver tumors? The probiotic Prohep is composed of Lactobacillus rhamnosus GG (LGG), Escherichia coli Nissle 1917 (EcN), and heat inactivated VSL#3 (1:1:1). VSL#3 contains: Streptococcus thermophilus, Bifidobacterium breve, Bifidobacterium longum, Bifidobacterium infantis, Lactobacillus acidophilus, Lactobacillus plantarum, Lactobacillus paracasei, and Lactobacillus delbrueckii. Note that Lactobacillus rhamnosus and some of the others are already found in many probiotic mixtures. From Medical Xpress:
Very exciting research IF it pans out - the idea of treating (some) cancers with probiotics (beneficial bacteria). This study was done on mice, and some mice started the probiotic mixture one week before they gave the mice the liver cancer, so...more limitations there. But the idea is so tantalizing and wonderful... And what was in the mixture of bacteria (called probiotic Prohep) that the mice ate that had beneficial results of shrinking liver tumors? The probiotic Prohep is composed of Lactobacillus rhamnosus GG (LGG), Escherichia coli Nissle 1917 (EcN), and heat inactivated VSL#3 (1:1:1). VSL#3 contains: Streptococcus thermophilus, Bifidobacterium breve, Bifidobacterium longum, Bifidobacterium infantis, Lactobacillus acidophilus, Lactobacillus plantarum, Lactobacillus paracasei, and Lactobacillus delbrueckii. Note that Lactobacillus rhamnosus and some of the others are already found in many probiotic mixtures. From Medical Xpress: The finding that the oral bacteria Streptococcus mutans, which is found in 10% of the population, is linked with hemorrhagic strokes is big. S. mutans is found in tooth decay or cavities (dental caries). The researchers found a link with cnm-positive S. mutans with both intracerebral hemorrhage (ICH) and also with cerebral microbleeds.
The finding that the oral bacteria Streptococcus mutans, which is found in 10% of the population, is linked with hemorrhagic strokes is big. S. mutans is found in tooth decay or cavities (dental caries). The researchers found a link with cnm-positive S. mutans with both intracerebral hemorrhage (ICH) and also with cerebral microbleeds.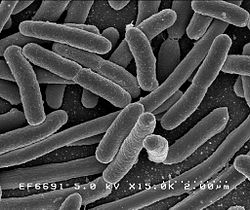 A recent study has examined the issue of whether the 10 to 1 ratio of bacteria to human cells, which is widely quoted, is actually correct. Weizmann Institute of Science researchers currently feel that based on scientific evidence (which of course will change over time) and making "educated estimates", the actual ratio is closer to 1:1 (but overall there still are more bacterial than human cells). They point out that the 10:1 ratio was originally a "back of the envelope" estimate dating back to 1972.
A recent study has examined the issue of whether the 10 to 1 ratio of bacteria to human cells, which is widely quoted, is actually correct. Weizmann Institute of Science researchers currently feel that based on scientific evidence (which of course will change over time) and making "educated estimates", the actual ratio is closer to 1:1 (but overall there still are more bacterial than human cells). They point out that the 10:1 ratio was originally a "back of the envelope" estimate dating back to 1972. This study is noteworthy and relevant to humans (it was done on mice) because it may explain why so many people taking antibiotics get frequent viruses or seem more susceptible to infections. Once bacteria (both good and bad) are killed by antibiotics, then the community becomes unbalanced (dysbiosis), so that viruses may gain a foothold and a viral infection develops. In a healthy microbial community all sorts of microbes can be found, even ones we typically consider pathogenic, but the whole community keeps them in balance. One can say that "depletion of commensal microbiota also affects antiviral immunity".
This study is noteworthy and relevant to humans (it was done on mice) because it may explain why so many people taking antibiotics get frequent viruses or seem more susceptible to infections. Once bacteria (both good and bad) are killed by antibiotics, then the community becomes unbalanced (dysbiosis), so that viruses may gain a foothold and a viral infection develops. In a healthy microbial community all sorts of microbes can be found, even ones we typically consider pathogenic, but the whole community keeps them in balance. One can say that "depletion of commensal microbiota also affects antiviral immunity". I posted about this amazing research while it was still ongoing (
I posted about this amazing research while it was still ongoing ( It's now 3 years being free of chronic sinusitis and off all antibiotics! Three amazing years since I started using easy do-it-yourself sinusitis treatments containing the probiotic (beneficial bacteria) Lactobacillus sakei. My sinuses feel great! And yes, it still feels miraculous.
It's now 3 years being free of chronic sinusitis and off all antibiotics! Three amazing years since I started using easy do-it-yourself sinusitis treatments containing the probiotic (beneficial bacteria) Lactobacillus sakei. My sinuses feel great! And yes, it still feels miraculous.
 This confirms what researchers such as
This confirms what researchers such as  Once again, two opposing views about beards have been in the news - that they harbor all sorts of nasty disease-causing bacteria vs they are hygienic. An earlier
Once again, two opposing views about beards have been in the news - that they harbor all sorts of nasty disease-causing bacteria vs they are hygienic. An earlier