![]() Eating several servings of seafood (especially fish) weekly has beneficial health effects throughout life, and now research finds another benefit in older adults. Seafood contains both EPA and DHA, which are two types of omega-3 fatty acids. DHA or docosahexanoic acid has "neuroprotective qualities" and is found in both the gray and white matter of the brain. Higher DHA levels (measured in the blood) was associated with better memory, less brain atrophy (better brain volume), and fewer amyloid plaques (which are associated with Alzheimer's) in cognitively healthy older adults. From Medscape:
Eating several servings of seafood (especially fish) weekly has beneficial health effects throughout life, and now research finds another benefit in older adults. Seafood contains both EPA and DHA, which are two types of omega-3 fatty acids. DHA or docosahexanoic acid has "neuroprotective qualities" and is found in both the gray and white matter of the brain. Higher DHA levels (measured in the blood) was associated with better memory, less brain atrophy (better brain volume), and fewer amyloid plaques (which are associated with Alzheimer's) in cognitively healthy older adults. From Medscape:
Higher Serum DHA Linked to Less Amyloid, Better Memory
New research supports neuroprotectant effects of docosahexaenoic acid (DHA) in the aging brain. In a small cross-sectional study of cognitively healthy older adults, higher serum DHA levels were associated with less cerebral amyloidosis, better memory scores, and less regional brain atrophy.
"The interesting finding was the association of low serum DHA levels with cerebral amyloidosis (amyloid plaques) in older adults without evidence of dementia," Hussein N. Yassine, MD, Department of Medicine, University of Southern California, Los Angeles, told Medscape Medical News. "This association was predominantly driven by persons at the lowest quartile of serum DHA levels who likely have limited intake of seafood." "This study adds to the existing evidence on the benefit of seafood consumption on [Alzheimer's disease] AD risk factors," Dr Yassine added.
The study was published online August 8 in JAMA Neurology. In a linked editorial, Joseph F. Quinn, MD, Department of Neurology, Oregon Health and Science University, Portland, notes that DHA is "the most abundant polyunsaturated fatty acid in the brain, playing an important structural role in synapses while also modulating a number of signaling pathways. "Brain DHA levels are also modulated by dietary intake, so it is plausible for dietary DHA to alter brain concentrations and affect downstream targets including brain pathology and function."
Dr Yassine and colleagues assessed serum DHA levels, measures of amyloid burden based on positron emission tomography with Pittsburgh compound B, brain volume, and neuropsychological test scores in 61 adults without dementia in the Aging Brain Study.
They found that serum DHA levels (percentage of total fatty acids) were 23% lower in those with cerebral amyloidosis relative to those without. Serum DHA levels were inversely correlated with brain amyloid load, independent of age, sex, years of education, and apolipoprotein E genotype. They also noted a positive correlation between serum DHA levels and brain volume in several subregions affected by AD, in particular the left subiculum and the left entorhinal volumes.
Clinically, there was a significant association between serum DHA levels and nonverbal memory. This association persisted after adjustment for age but not after adjustment for apolipoprotein E genotype. Serum DHA levels were not associated with measures of global cognition, executive function, or verbal memory scores.

 Yes! Treating young children who have peanut allergies with doses of
Yes! Treating young children who have peanut allergies with doses of  Again, another study showing the importance of lifestyle factors in the development of protein buildups in the brain that are associated with the onset of Alzheimer's disease. Specifically, the study found that each one of several lifestyle factors—a healthy body mass index, physical activity and a Mediterranean diet, were linked to lower levels of plaques and tangles on brain scans in people who already had mild memory changes, (but not dementia). Other posts discussing Mediterranean diet and brain health (brain volume, etc.) are
Again, another study showing the importance of lifestyle factors in the development of protein buildups in the brain that are associated with the onset of Alzheimer's disease. Specifically, the study found that each one of several lifestyle factors—a healthy body mass index, physical activity and a Mediterranean diet, were linked to lower levels of plaques and tangles on brain scans in people who already had mild memory changes, (but not dementia). Other posts discussing Mediterranean diet and brain health (brain volume, etc.) are  Two recent articles about BPA (bisphenol A), BPS (bisphenol B), and the "BPA-free" label - one a study, and one a review article. The "BPA-free" label unfortunately means the product contains a product similar to BPA (typically BPS) and with the same problems as BPA. Both articles discuss the accumulating health reasons to try to avoid these endocrine disruptors. Which is really , really tough to do given that plastics are all around us and used by us every day.
Two recent articles about BPA (bisphenol A), BPS (bisphenol B), and the "BPA-free" label - one a study, and one a review article. The "BPA-free" label unfortunately means the product contains a product similar to BPA (typically BPS) and with the same problems as BPA. Both articles discuss the accumulating health reasons to try to avoid these endocrine disruptors. Which is really , really tough to do given that plastics are all around us and used by us every day. Earlier posts discussed research that showed that farm and animal (pets such as dogs) exposures in the first year of life is protective against allergies and asthma (lowers the risk of developing them).
Earlier posts discussed research that showed that farm and animal (pets such as dogs) exposures in the first year of life is protective against allergies and asthma (lowers the risk of developing them).  The
The  Get active, really active, to reduce your risk for 5 diseases: breast cancer, colon cancer, heart disease, and ischemic stroke. Instead of the 150 minutes of brisk walking or 75 minutes per week of running (which is equal to the 600 metabolic equivalent (MET) minutes now recommended by the World Health Organization), this study found that much more exercise is needed for
Get active, really active, to reduce your risk for 5 diseases: breast cancer, colon cancer, heart disease, and ischemic stroke. Instead of the 150 minutes of brisk walking or 75 minutes per week of running (which is equal to the 600 metabolic equivalent (MET) minutes now recommended by the World Health Organization), this study found that much more exercise is needed for 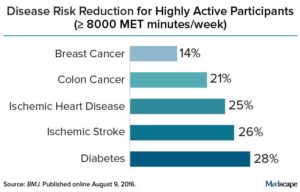 Credit: Medscape
Credit: Medscape Take note: what is happening to dogs is also happening to men. Specifically, for many decades - year by year - there has been a decrease in male dog fertility. And yes, this is also happening with human male fertility - a decline in male semen quality (including sperm), along with an increase in the incidence of testicular cancer, the birth defect hypospadias, and undescended testes. This cluster of problems is called testicular dysgenesis syndrome (TGS
Take note: what is happening to dogs is also happening to men. Specifically, for many decades - year by year - there has been a decrease in male dog fertility. And yes, this is also happening with human male fertility - a decline in male semen quality (including sperm), along with an increase in the incidence of testicular cancer, the birth defect hypospadias, and undescended testes. This cluster of problems is called testicular dysgenesis syndrome (TGS Another study reporting health benefits of drinking tart cherry juice, specifically in speeding recovery following prolonged, repeat sprint activity (think soccer and rugby). The researchers found that after a prolonged, intermittent sprint activity, the cherry juice significantly lowered levels of Interleukin-6, a marker for inflammation and that there was a decrease in muscle soreness. The study participants drank the cherry juice (1 oz cherry juice concentrate mixed with 100 ml water) for several days before and several days after the sprint activity. Montmorency tart cherry juice is a
Another study reporting health benefits of drinking tart cherry juice, specifically in speeding recovery following prolonged, repeat sprint activity (think soccer and rugby). The researchers found that after a prolonged, intermittent sprint activity, the cherry juice significantly lowered levels of Interleukin-6, a marker for inflammation and that there was a decrease in muscle soreness. The study participants drank the cherry juice (1 oz cherry juice concentrate mixed with 100 ml water) for several days before and several days after the sprint activity. Montmorency tart cherry juice is a