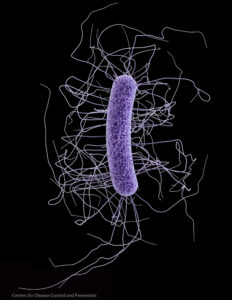
 Important new research was published in January 2016 about a fecal microbiota transplant (FMT) or "poop transplant". The research compared only one patient's gut microbes (thus a case study) to her fecal transplant donor's gut microbes, but it is important for looking at how gut microbes change long-term after a fecal microbiota transplant (poop transplant) and the actual length of time that it takes for the recipient's gut microbial community to become like the donor's gut microbiome. The patient was quickly "cured" of a serious recurrent Clostridium difficile infection after one fecal micriobiota transplant (FMT) from her sister, but there were ongoing long-term changes in the patient's gut microbes for 4.5 years, at which point the microbes (bacteria and viruses) were like the donor's (at the phylum, class, and order levels), and with similar bacterial diversity. At this point the researchers said that "full engraftment" of microbes had occurred.
Important new research was published in January 2016 about a fecal microbiota transplant (FMT) or "poop transplant". The research compared only one patient's gut microbes (thus a case study) to her fecal transplant donor's gut microbes, but it is important for looking at how gut microbes change long-term after a fecal microbiota transplant (poop transplant) and the actual length of time that it takes for the recipient's gut microbial community to become like the donor's gut microbiome. The patient was quickly "cured" of a serious recurrent Clostridium difficile infection after one fecal micriobiota transplant (FMT) from her sister, but there were ongoing long-term changes in the patient's gut microbes for 4.5 years, at which point the microbes (bacteria and viruses) were like the donor's (at the phylum, class, and order levels), and with similar bacterial diversity. At this point the researchers said that "full engraftment" of microbes had occurred.
Until 7 months post-FMT, the patient's microbial communities varied over time and showed little overall similarity to the donor, indicating "ongoing gut microbiota adaption" during the first seven months. But right after the transplant, the changes were enough for the patient to be immediately "cured" of her recurrent Clostridium difficile infection. The long-term results also suggested that phages (viruses) may play an important role in gut health. From Cold Spring Harbor Molecular Case Studies:
Fecal microbiota transplantation (FMT) is an effective treatment for recurrent Clostridium difficile infections (RCDIs). However, long-term effects on the patients’ gut microbiota and the role of viruses remain to be elucidated. Here, we characterized bacterial and viral microbiota in the feces of a cured RCDI patient at various time points until 4.5 yr post-FMT compared with the stool donor. Feces were subjected to DNA sequencing to characterize bacteria and double-stranded DNA (dsDNA) viruses including phages.
The patient's microbial communities varied over time and showed little overall similarity to the donor until 7 mo post-FMT, indicating ongoing gut microbiota adaption in this time period. After 4.5 yr, the patient's bacteria attained donor-like compositions at phylum, class, and order levels with similar bacterial diversity. Differences in the bacterial communities between donor and patient after 4.5 yr were seen at lower taxonomic levels.
C. difficile remained undetectable throughout the entire time span. This demonstrated sustainable donor feces engraftment and verified long-term therapeutic success of FMT on the molecular level. Full engraftment apparently required longer than previously acknowledged, suggesting the implementation of year-long patient follow-up periods into clinical practice. The identified dsDNA viruses were mainly Caudovirales phages. Unexpectedly, sequences related to giant algae–infecting Chlorella viruses were also detected. Our findings indicate that intestinal viruses may be implicated in the establishment of gut microbiota.
FMT has shown impressive success rates of ∼90% against RCDIs and no severe adverse effects (Gough et al. 2011; Cammarota et al. 2014; O'Horo et al. 2014).... FMT led to increased donor-like intestinal bacterial diversities within 2 wk (van Nood et al. 2013).....Because viruses, especially phages, are the most abundant intestinal entities with the ability to influence microbial communities (Barr et al. 2013; Virgin 2014), they may well be relevant to C. difficile infection and the microbial changes following FMT.
Briefly, the female patient was 51 years old when admitted to the University Hospital of Zurich with her sixth episode of RCDI, suffering from severe diarrhea and weight loss.....Following FMT, the patient reported changes in bowel movements and intermittent obstipation, both of which ceased within 10 wk. Ever since, the patient has remained free of symptoms for almost 5 yr now..
The analysis of viral dsDNA sequences reported earlier revealed the presence of 22 viruses throughout samples D0, P1, P2, and P3 . In each sample, eight to 11 different viruses were identified, mainly belonging to the Caudovirales order (tailed dsDNA phages) that contains the viral families Myo-, Podo-, and Siphoviridae. Most viruses, 14 of 22, were identified uniquely in either sample. Three phages, the Erwinia phage vB_EamP-L1 (Podoviridae) and the two Bacteroides phages B124-14 and B40-8 (Siphoviridae), were consistently detected in all four samples and each contained phages of all three Caudovirales groups.
The bacterial composition of the donor was relatively stable and comparable at the time of FMT and 4.5 yr later (Fig. 1B), which is in accordance with the known temporal stability of adult intestinal microbiota (Zoetendal et al. 1998)....The patient's fecal microbiota underwent extensive compositional fluctuations and were dominated by Firmicutes up to 7 mo post-FMT, suggesting ongoing adaptation processes of donor microbiota in the patient's intestine that may also reflect changes in nutrition over the observation period. This is in accordance with our and other groups’ recent findings that showed high degrees of bacterial variation in RCDI patients up to 7 mo post-FMT (Broecker et al. 2013; Weingarden et al. 2015).
However, 4.5 yr post-FMT, the patient's bacteria have attained a donor-like composition at the phylum level, indicating full and stable engraftment of the donor's microbiota.....Of note, four of the five most prominent genera identified in both donor samples as well as the patient sample after 4.5 yr, Alistipes, Bacteroides, Dialister, and Faecalibacterium (Fig. 1D), are known constituents of healthy fecal microbiota (Claesson et al. 2011; Joossens et al. 2011). This further indicated that FMT led to healthy and sustainable microbiota in the patient.
One notable species detected in these three samples is Faecalibacterium prausnitzii (Fig. 1D). This species was also detected in the patient samples 6–7 mo post-FMT with abundances of <0.1% (data not shown). Faecalibacterium prausnitzii is recognized as one of the most important species of healthy individuals and normally constitutes >5% of the gut microbiota (Miquel et al. 2013).
The fact that the patient's clinical symptoms, which included severe diarrhea in the absence of antibiotic treatment against C. difficile (Broecker et al. 2013), resolved promptly after FMT suggests that gut microbiota were able to exert normal metabolic functions even before full engraftment. This may be explained by the fact that the patient's bacterial diversity even during the highly variable time period up to 7 mo post-FMT was already in the range of the healthy donor. In agreement with the absence of symptoms until today, C. difficile bacteria were undetectable in the samples of the patient, similar to the donor who tested negative for C. difficile before FMT.....The finding that the patient's fecal microbiota attained a highly donor-like composition after 4.5 yr suggests that long-term follow-up should be implemented into clinical practice.
The analysis of viral dsDNA sequences from a previous study revealed the presence of Caudovirales phages in all investigated samples of the donor and the patient. Caudovirales have been shown before to be the dominant viruses in the human intestine, followed by ssDNA phages of the Microviridae family that we were unable to detect with the metagenomic sequencing approach (Lepage et al. 2008; Norman et al. 2015). Three phages were identified in all of the analyzed samples of the donor and the patient.

 More research that supports that both more variety (diversity) of microbes and the actual mix of types of microbes are involved in a healthy
More research that supports that both more variety (diversity) of microbes and the actual mix of types of microbes are involved in a healthy