 A nice summary article about the benefits and risks of coffee consumption. Summary of effects of drinking coffee: 1) May potentially increase blood pressure, but also may lower the risk for coronary disease, and protect against heart disease. 2) May cut stroke risk by as much as 25%, 3) Linked to improved glucose metabolism, reduced risk for type 2 diabetes, and promotion of weight loss in overweight patients. 4) May reduce the risk for several cancers. 5) Appears to slow the progression of dementia and Parkinson's disease. 6) A significantly decreased risk of developing depression. 7) Slows progression in alcoholic cirrhosis, hepatitis C, and NAFLD (non-alcoholic fatty liver disease). 8) May be beneficial in dry-eye syndrome, gout, and in preventing MRSA infection. 9) May increase blood pressure, anxiety, insomnia, tremor, withdrawal symptoms, and potential increased risk of glaucoma. From Medscape:
A nice summary article about the benefits and risks of coffee consumption. Summary of effects of drinking coffee: 1) May potentially increase blood pressure, but also may lower the risk for coronary disease, and protect against heart disease. 2) May cut stroke risk by as much as 25%, 3) Linked to improved glucose metabolism, reduced risk for type 2 diabetes, and promotion of weight loss in overweight patients. 4) May reduce the risk for several cancers. 5) Appears to slow the progression of dementia and Parkinson's disease. 6) A significantly decreased risk of developing depression. 7) Slows progression in alcoholic cirrhosis, hepatitis C, and NAFLD (non-alcoholic fatty liver disease). 8) May be beneficial in dry-eye syndrome, gout, and in preventing MRSA infection. 9) May increase blood pressure, anxiety, insomnia, tremor, withdrawal symptoms, and potential increased risk of glaucoma. From Medscape:
How Healthy Is Coffee? The Latest Evidence
Earlier this year, the Dietary Guidelines Advisory Committee (DGAC) released a report[1] stating that up to five cups of coffee per day, or up to 400 mg of caffeine, is not associated with long-term health risks. Not only that, they highlighted observational evidence that coffee consumption is associated with reduced risk for several diseases, including type 2 diabetes, cardiovascular disease (CVD), and neurodegenerative disorders. The body of data suggesting that moderate coffee—and, in all likelihood, tea—consumption is not only safe but beneficial in a variety of mental and medical conditions is growing fast.
A 2012 study of over 400,000 people, published in the New England Journal of Medicine, reported that coffee consumption is associated with a 10% reduction in all-cause mortality at 13-year follow-up.... It's important to note that much of the evidence on the potential health effects of coffee, caffeine, and other foods and nutrients is associational and doesn't prove causality—observational investigations come with limitations and often rely on error-prone methods such as patient questionnaires. However, the sheer volume of existing observational data linking coffee and/or caffeine with various health benefits—as well as, in many cases, evidence of a dose response—suggests that the most widely consumed stimulant in the world has positive influences on our health.
Cardiovascular Disease:...However, when caffeine is ingested via coffee, enduring blood pressure elevations are small and cardiovascular risks may be balanced by protective properties. Coffee beans contain antioxidant compounds that reduce oxidation of low-density lipoprotein (LDL) cholesterol, and coffee consumption has been associated with reduced concentrations of inflammatory markers. Moderate coffee intake is associated with a lower risk for coronary heart disease as far out as 10 years, and data suggest that an average of two cups per day protects against heart failure.
Cerebrovascular Disease and Stroke: The vascular benefits of coffee are not lost on the brain. According to a 2011 meta-analysis, consuming between one and six cups per day reportedly cut stroke risk by 17%. A 22%-25% risk reduction was seen in a large sample of Swedish women followed for an average of 10 years.
Diabetes:...Numerous studies have linked regular coffee drinking with improved glucose metabolism, insulin secretion, and a significantly reduced risk for diabetes. Most recently, findings from a long-term study published this year suggest that coffee drinkers are roughly half as likely to develop type 2 diabetes as are nonconsumers, even after accounting for smoking, high blood pressure, and family history of diabetes.
Cancer: ...Evidence suggests that moderate to heavy coffee consumption can reduce the risk for numerous cancers, including endometrial (> 4 cups/day), prostate (6 cups/day), head and neck (4 cups/day), basal cell carcinoma (> 3 cups/day), melanoma,and breast cancer (> 5 cups/day). The benefits are thought to be at least partially due to coffee's antioxidant and antimutagenic properties.
Neurodegeneration: Beyond the short-term mental boost it provides, coffee also appears to benefit longer-term cognitive well-being. A 2012 study reported that patients with mild cognitive impairment and plasma caffeine levels of > 1200 ng/mL—courtesy of approximately three to five cups of coffee per day—avoided progression to dementia over the following 2-4 years. On a related note, a study from last year reported that caffeine consumption appears to enhance memory consolidation....Caffeinated coffee has long been thought to be neuroprotective in Parkinson disease (PD)....—as well as in multiple sclerosis.
Depression: A 2011 study suggests that a boost in coffee consumption might also benefit our mental health: Women who drank two to three cups of coffee per day had a 15% decreased risk for depression compared with those who drank less than one cup per week. A 20% decreased risk was seen in those who drank four cups or more per day. Newer work also suggests that regular coffee drinking may be protective against depression.
Liver Disease: The liver might help break down coffee, but coffee might protect the liver (in some cases). Evidence suggests that coffee consumption slows disease progression in patients with alcoholic cirrhosis and hepatitis C, and reduces the risk of developing hepatocellular carcinoma. A 2012 study reported that coffee intake is associated with a lower risk for nonalcoholic fatty liver disease (NAFLD), while work published in 2014 found that coffee protects against liver fibrosis in those with already established NAFLD.
And That's Not All…: An assortment of other research suggests that coffee intake might also relieve dry-eye syndrome by increasing tear production, reduce the risk for gout, and potentially fight infection. Coffee and hot tea consumption were found to be protective against one of the medical community's most concerning bugs, methicillin-resistant Staphylococcus aureus (MRSA). While it remains unclear whether the beverages have systemic antimicrobial activity, study participants who reported any consumption of either were approximately half as likely to have MRSA in their nasal passages.
And Finally, the Risks: As is often the case, with benefits come risks, and coffee consumption certainly has negative medical and psychiatric effects to consider. Besides the aforementioned potential increase in blood pressure, coffee can incite or worsen anxiety, insomnia, and tremor and potentially elevate glaucoma risk. Also, given the potential severity of symptoms, caffeine withdrawal syndrome is included as a diagnosis in the DSM-5.
 It turns out that people experiencing a major depression have differences in their gut microbiome (community of microbes) when compared to healthy people who are not depressed. A persistent and prolonged period of extreme sadness or depression is called a major depressive disorder (MDD).
It turns out that people experiencing a major depression have differences in their gut microbiome (community of microbes) when compared to healthy people who are not depressed. A persistent and prolonged period of extreme sadness or depression is called a major depressive disorder (MDD).
 Disappointing results from a large
Disappointing results from a large  This actually may seem obvious to many: that older people cope better in terms of loneliness and depression after a spouse's death or divorce if they have at least 1 pet cat or dog (versus no pets), but it's good to read that an
This actually may seem obvious to many: that older people cope better in terms of loneliness and depression after a spouse's death or divorce if they have at least 1 pet cat or dog (versus no pets), but it's good to read that an  A number of recent studies and articles have discussed the effectiveness of diet in treating or preventing depression with the main conclusion that yes, it helps. Now an observational study (that will be presented in April) found that elderly people following the DASH diet most closely were 11% less likely to become depressed over time than those that did not.
A number of recent studies and articles have discussed the effectiveness of diet in treating or preventing depression with the main conclusion that yes, it helps. Now an observational study (that will be presented in April) found that elderly people following the DASH diet most closely were 11% less likely to become depressed over time than those that did not. A newly published study suggests that exercising an hour or more per week could lower the incidence of depression.
A newly published study suggests that exercising an hour or more per week could lower the incidence of depression. 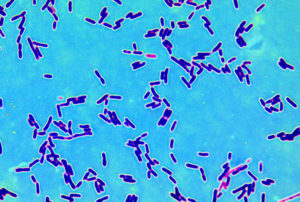 Could probiotics be used to treat depression? The medical site Medscape reported on a very small preliminary study (only 10 people) that tested that idea, with findings that suggested that taking certain probiotics does help treat the symptoms of mild to moderate depression. The bacteria taken were Lactobacillus helveticus and Bifidobacterium longum (in the product Probio'Stick). Specifically, the symptoms of mood, anhedonia (inability to feel pleasure), and sleep disturbance were significantly reduced after probiotoc therapy.
Could probiotics be used to treat depression? The medical site Medscape reported on a very small preliminary study (only 10 people) that tested that idea, with findings that suggested that taking certain probiotics does help treat the symptoms of mild to moderate depression. The bacteria taken were Lactobacillus helveticus and Bifidobacterium longum (in the product Probio'Stick). Specifically, the symptoms of mood, anhedonia (inability to feel pleasure), and sleep disturbance were significantly reduced after probiotoc therapy. Perhaps a nutrient deficit is associated with depression? This study found that eating a Mediterranean diet or a similar diet in which fruits, vegetables, legumes (beans), nuts, and low in processed meats is associated with lower rates of depression. From Medical Xpress:
Perhaps a nutrient deficit is associated with depression? This study found that eating a Mediterranean diet or a similar diet in which fruits, vegetables, legumes (beans), nuts, and low in processed meats is associated with lower rates of depression. From Medical Xpress: