![]() More reasons to eat a variety of foods - each food will contribute something different, and the effects may be subtle. Here are two healthy foods from plants: orange juice and shiitake mushrooms. From Medical Xpress
More reasons to eat a variety of foods - each food will contribute something different, and the effects may be subtle. Here are two healthy foods from plants: orange juice and shiitake mushrooms. From Medical Xpress
Orange juice could help improve brain function in elderly people
Drinking orange juice could help improve brain function in elderly people, according to new research from the University of Reading.The study saw a group of 37 healthy adults (mean age 67 years) consuming 500 ml (just under a pint) of orange juice, daily over an eight week period. At the beginning and end of the eight weeks their memory, reaction time and verbal fluency was measured. These were then combined into one overall score known as 'global cognitive function'. The adults showed an 8% overall improvement in global cognitive function after orange juice consumption compared to a control drink (matched for taste and calories) given during a different eight week period. Although subtle, these improvements are significant. ."
Orange juice is a major source of a group of naturally occurring plant phytochemicals known as flavonoids, being particularly rich in a sub-class of flavonoids, known as flavanones. Recent studies from the School of Chemistry, Food and Pharmacy have shown that flavonoids may improve memory through the activation of signalling pathways in the hippocampus, a part of the brain that is associated with learning and memory.
Previous Reading research has shown that other flavonoid rich foods such as blueberries are beneficial for cognition. Research is still ongoing to determine the exact mechanisms by which flavonoids may exert benefits to the brain. Several mechanisms haveboosting immune systbeen proposed such as improved blood flow in the brain and protecting neurons against oxidative damage and increasing the efficiency with which neurons transmit signals.
This study was published in April 2015, from Science Daily: Mushrooms boost immunity, suggests research
Could a mushroom a day help keep the doctor away? A new University of Florida study shows increased immunity in people who ate a cooked shiitake mushroom every day for four weeks.... 52 healthy adults, age 21 to 41, came to the Gainesville campus, where researchers gave them a four-week supply of dry shiitake mushrooms. Participants took the mushrooms home, cleaned and cooked them. Then they ate one, 4-ounce serving of mushrooms each day during the experiment. Through blood tests before and after the experiment, researchers saw better-functioning gamma delta T-cells and reductions in inflammatory proteins.
"If you eat a shiitake mushroom every day, you could see changes in their immune system that are beneficial," said Percival, an Institute of Food and Agricultural Sciences faculty member. "We're enhancing the immune system, but we're also reducing the inflammation that the immune system produces."

 My last post was about a recent Medscape article discussing whether
My last post was about a recent Medscape article discussing whether 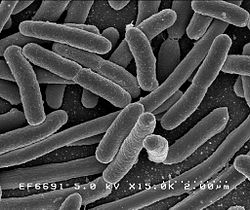 How does the medical profession currently view probiotics in the prevention and treatment of urinary tract infections (UTIs), especially recurrent infections? Answer: Only a few studies have been done, but what little is known is promising, which is good because traditional antibiotic treatment has problems (especially antibiotic resistance).
How does the medical profession currently view probiotics in the prevention and treatment of urinary tract infections (UTIs), especially recurrent infections? Answer: Only a few studies have been done, but what little is known is promising, which is good because traditional antibiotic treatment has problems (especially antibiotic resistance). In a newly published study looking at how infant gut microbes change over time, once again babies had differences in gut bacteria depending on whether they were delivered vaginally or by Cesarean section.
In a newly published study looking at how infant gut microbes change over time, once again babies had differences in gut bacteria depending on whether they were delivered vaginally or by Cesarean section. Amusing but also scary. The negative effects on the gut microbes of one person consuming an all fast food diet for 10 days occurred very quickly, and his gut microbes did not recover even 2 weeks after the fast food diet ended. Biggest problem seemed to be loss of gut diversity - about 40% of his gut bacterial species. Loss of gut diversity is considered a sign of ill health. Written by Tim Spector, with Tom Spector's assistance, from The Conversation:
Amusing but also scary. The negative effects on the gut microbes of one person consuming an all fast food diet for 10 days occurred very quickly, and his gut microbes did not recover even 2 weeks after the fast food diet ended. Biggest problem seemed to be loss of gut diversity - about 40% of his gut bacterial species. Loss of gut diversity is considered a sign of ill health. Written by Tim Spector, with Tom Spector's assistance, from The Conversation:
 Tom Spector. Credit: Tim Spector
Tom Spector. Credit: Tim Spector More studies need to be done, but the possibility of simply taking 500 mg twice a day of
More studies need to be done, but the possibility of simply taking 500 mg twice a day of 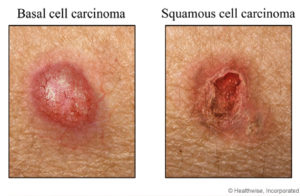 Credit: WebMD, Healthwise, Inc.
Credit: WebMD, Healthwise, Inc. Controversy exists over whether healthy people should take
Controversy exists over whether healthy people should take  Another piece of research that shows that eating
Another piece of research that shows that eating